Submission to the College of Physicians and Surgeons of
Saskatchewan
(5 June, 2015)
Re: Conscientious Refusal
(as revised)
Appendix "A"
Ontario College briefing materials
Full Text

A1. Introduction
A1.1 The Council of the College of Physicians and
Surgeons of Ontario (CPSO) was provided with a briefing note by the working
group that drafted Professional Obligations and Human Rights. The
briefing note helped to convince the Council to approve the policy.
A1.2 However, a review of the briefing materials shows
them to be deficient, erroneous and seriously misleading. Moreover, it
appears to have been physically impossible for the working group to have
considered the results of the second public consultation before preparing
the briefing materials.
A1.3 This suggests that the Saskatchewan College
Council should give little weight to the CPSO briefing note and not rely
upon the information it provides without independently verifying it, if
possible.
A2. Citation of Conscientious Refusal (CR No.1)
A2.1 One of the reasons offered by the working group to
justify the policy, including a requirement for compulsory referral, was
that it aligned with "the position taken by the College of Physicians and
Surgeons of Saskatchewan (CPSS) in their draft policy titled Conscientious
Refusal" and had been "approved in principle by the CPSS Council."
A2.2 This was clearly premature, since Conscientious
Refusal no longer aligns with the Ontario policy, and the withdrawal of the
requirement for referral supports the view that the CPSO requirement of
"effective referral" is unacceptable. (III.1)
A3. Reasonable apprehension of bias
A3.1 The Christian Medical and Dental Society and the
Canadian Federation of Catholic Physicians' Societies have filed an
application in the Ontario Superior Court of Justice asking for an
injunction against enforcement of the CPSO policy, Professional
Obligations and Human Rights.1
A3.2 According to the application, the CPSO
acknowledged that it had received 15,977 submissions during the second
consultation concerning the policy, which ended on 20 February, 2015. The
great majority of submissions opposed the policy.
A3.3 While the consultation ended on 20 February, a
working group wrote the final version of the policy by 11 February, at least
nine days before the consultation closed. This is one of the
factors that gives rise to concern about what the CMDS application calls
either "actual bias" or "a reasonable apprehension of bias" on the part of
the working group.
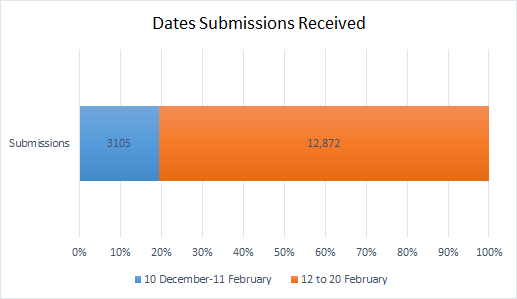
A3.4 On this point, the statistics provided by the CPSO
are of interest.
A3.5 According to the briefing note supplied to the
College Council,2 by 11 February, 2015
the College had received 3,105 submissions. This means that 12,872
submissions were received from 12 to 20 February inclusive. In other words,
over 80% of the submissions in the second consultation were received
after the final version of the policy had been written.
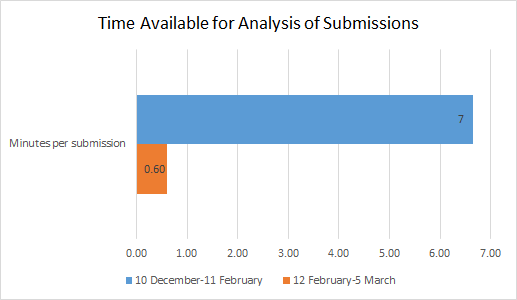
A3.6 Moreover, allowing sufficient time to receive
feedback is only the beginning. Having received them, one would expect that
a working group seriously interested in feedback would allow sufficient time
to review and analyse the submissions.
A3.7 During the 64 days of consultation ending 11
February, the College received an average of almost 50 submissions per day.
There were 43 working days during that period. Assuming someone spent eight
full hours every working day reading the submissions, it would have taken
one person about seven minutes to review each one.
A3.8 However, the College received an average of one
submission every minute of every hour of the last nine days of consultation
ending 20 February. With 16 working days available from 12 February to 5
March inclusive, the day before the Council meeting, one person reading
eight hours a day would have had no more than 36 seconds to review each
submission.
A3.9 This demonstrates that it is highly unlikely that
the CPSO briefing note can be safely relied upon by the Saskatchewan
College.
A4. Tunnel Vision at the College of Physicians*
A4.1 The College of Physicians and Surgeons of Ontario
has adopted a policy requiring physicians who have moral or ethical
objections to a procedure to make an "effective referral" of patients to a
colleague who will provide it, or to an agency that will arrange for it.3
In 2008, amidst great controversy,4 the
Australian state of Victoria passed an abortion law with a similar
provision.5
A4.2 After the law passed, a Melbourne physician,
morally opposed to abortion, publicly announced that he had refused to
provide an abortion referral for a patient. This effectively challenged the
government and medical regulator to prosecute or discipline him. They did
not. The law notwithstanding, no one dared prosecute him for refusing to
help a woman 19 weeks pregnant obtain an abortion because she and her
husband wanted a boy, not a girl.
A4.3 They obtained the abortion without the assistance
of the objecting physician,6 and they
could have done the same in Ontario. College Council member Dr. Wayne
Spotswood, himself an abortion provider, told Council that everyone 15 or 16
years old knows that anyone refused an abortion by one doctor "can walk down
the street" to obtain the procedure elsewhere.7
A4.4 So why did the College working group that drafted
the demand for "effective referral" urge College Council to adopt a policy
that so clearly has the potential to make the College look ridiculous?
A4.5 Moreover, why did the working group push for a
policy of "effective referral" despite having no evidence that even a single
person in Ontario has ever been unable to access medical services because of
conscientious objection by a physician?8
A4.6 Why did the working group supply Council with
deficient, erroneous and seriously misleading briefing materials9
- falsely implying, for example, that the Australian Medical Association
supports "effective referral" by objecting physicians?10
A4.7 Having selected the American Medical Association
for purposes of policy comparison, why did the working group fail to cite
any AMA policy document in its December briefing materials,11
and then, in March, leave out12 the fact
that AMA policy does not require "effective referral"?13
If AMA policy was relevant in 2014, why was it irrelevant in 2015?
A4.8 College consultation policy states that it "does
not review any content of any feedback for accuracy."14
Why, then, did the working group intervene in the second public consultation
discussion forum, trying to stifle contributors' criticism by offering a
purportedly 'correct' interpretation of the policy?15
A4.9 Why did the working group make final revisions to
the draft policy nine days before the second public consultation
closed, dismissing opposition that was overwhelming even then?16
A4.10 Four months elapsed between the end of the first
public consultation and the working group's first report and recommendations
to Council.17 In contrast, Council was
asked to pass the policy two weeks after the close of the second
consultation. Why the rush?18
A4.11 And why did the working group wait until the day
before the meeting to supply Council members with an explanation of the new
policy?19 Why has it not, even yet,
published a report of the second on-line survey like that provided during
the first?
A4.12. Lack of knowledge, lack of foresight, poor
judgement, poor research, human error and carelessness might explain these
problems, but for one disturbing fact. Almost every one of the errors,
omissions, and deficiencies and every active intervention or decision made
by the working group favoured its "effective referral" policy.
A4.13 What we seem to have here is not merely a series
of unfortunate events, but a pattern of conduct strongly suggestive of a
narrow and fixed ideological bias.
A4.14 Why such an impractical policy? Why insist upon
it when there is no evidence to support it? Why the deficiencies, errors and
misleading statements? Why finalize the policy nine days before the
consultation ended? Why call for an immediate decision about a controversial
policy affecting fundamental freedoms, without time for reflection - without
even a complete accounting of the second consultation?
A4.15 The most cogent answer is that the working group,
if not blinded by ideological extremism, had an exceptionally bad case of
tunnel vision.
A4.16 Tunnel vision explains why the working group
thought it a concession to allow a physician to refer a woman seeking a
sex-selective abortion to an "agency" that would arrange for it rather than
a physician who would provide it.
A4.17 Exceptionally bad tunnel vision accounts for the
suggestion by the chairman of the working group and the president of the
College that doctors opposed to abortion can avoid compromising their
beliefs by sending patients with unwanted pregnancies to abortion clinics.20
A4.18 But there is yet no satisfactory explanation for
the policy's central message: that ethical medical practice requires
physicians to do what they believe to be unethical. Even the worst
imaginable case of tunnel vision cannot account for that kind of incoherent
authoritarianism.
A4.19 The working group failed to provide any evidence
that the suppression of fundamental freedoms entailed by Professional
Obligations and Human Rights was justified, and that no less
restrictive means were available to achieve the legitimate objectives of the
College. Despite this - and without seriously considering any of the
foregoing questions - College Council approved the policy. If this is not
the best possible example of blind faith by institutional decision makers,
it will do until a better one comes along.
A4.20 Having failed to consider these questions before
approving Professional Obligations and Human Rights, it appears
that College Council will soon have the opportunity to consider them again.
Indeed, the Council may be compelled to answer them - not in the closely
controlled and congenial environment of its own offices, but in open court
during a lawsuit launched by the Christian Medical Dental Society. That will
likely be the beginning of a long trek to the Supreme Court of Canada, one
that could have been avoided had College Council properly discharged its
responsibilities.
A4.21 Certainly, the College is obliged "to protect and
serve the public interest."21 But the
public interest is served by civility, restraint, tolerance, accommodation
of divergent views and respect for fundamental freedoms. That requires
broad-mindedness and evidence-based decision-making, not tunnel vision and
blind faith.
*This appeared as an op-ed column in the
National Post on 13 April, 2015. It is reproduced here in
numbered paragraphs, with the notes not published with the column.
Notes
1. Ontario Superior Court of Justice, Between the
Christian Medical and Dental Society of Canada et al and College of Physicians
and Surgeons of Ontario,
Notice of
Application, 20 March, 2015. Court File 15-63717 ()
2. Salte BE.
Memorandum
to Council re: Draft Policy- Conscientious Objection, 23 March,
2015 (CPSS No. 75/15) p. 4-11.
3. College of Physicians and Surgeons of Ontario,
Professional Obligations and Human Rights (Accessed
2015-03-22)
4.
Letter from Dr. Mark Hobart to Mr. Edward O'Donohue, Chairperson, Scrutiny
of Acts and Regulation Committee, Parliament of Victoria, dated 7 June,
2011. (Accessed 2015-02-19).
5. Murphy S.
"State of Victoria, Australia
demands referral, performance of abortions: Abortion Law Reform Act 2008."
Protection of Conscience Project
6. Rolfe P.
"Melbourne doctor's abortion stance may be punished." Herald Sun,
28 April, 2013 (Accessed 2015-02-19); Devine M.
"Doctor risks his career after refusing abortion referral." Herald Sun,
5 October, 2013 (Accessed 2015-02-19).
7. Swan M.
"UPDATED: Ontario doctors must refer for abortions, says College of
Physicians." The Catholic Register, 6 March, 2015 (Accessed
2015-03-10).
8. Protection of Conscience Project, Submission
to the College of Physicians and Surgeons of Ontario Re: Professional
Obligations and Human Rights (20 February, 2015),
Appendix
"D".
9. Protection of Conscience Project, Submission
to the College of Physicians and Surgeons of Ontario Re: Professional
Obligations and Human Rights (20 February, 2015),
Appendix
"B": Unreliability of Jurisdictional Review by College Working Group.
10. Protection of Conscience Project, Submission
to the College of Physicians and Surgeons of Ontario Re: Professional
Obligations and Human Rights (20 February, 2015),
Appendix "B": Unreliability of Jurisdictional Review by College Working
Group- BII.3 (Australia)
11. It quoted a single sentence referring
generally to AMA policy from an article about conscientious objection among
pharmacists. Protection of Conscience Project Submission to the College of
Physicians and Surgeons of Ontario Re: Professional Obligations and Human
Rights (20 February, 2015),
Appendix "B": Unreliability of Jurisdictional Review by College Working
Group- BII.5.1 (USA)
12. Council Briefing Note-
Topic: Professional Obligations and Human Rights- Consultation Report and
Revised Draft Policy (March, 2015). In Meeting of Council, March 6,
2015, p 60-67(Accessed 2015-03-23).
13.
Letter from the AMA Council of Ethical and Judicial Affairs to the College
of Physicians and Surgeons of Ontario, 18 February, 2015 (Accessed
2015-03-23)
14. College of Physicians and Surgeons of
Ontario,
The Consultation Process and Posting Guidelines. (Accessed
2015-03-22).
15. Murphy S.
"A watchdog in need of a leash." Protection of Conscience Project
Blog, 3 February, 2015.
16. College of Physicians and Surgeons of
Ontario,
Meeting of Council 6 March, 2015, p. 61. (Accessed 2015-03-23)
17. The first consultation closed on 5 August,
2014. The meeting occurred 4-5 December, 2014.
18. The second consultation closed 20 February,
2015. Council was asked to pass the policy on 6 March, 2015.
19. Swan M.
"UPDATED: Ontario doctors must refer for abortions, says College of
Physicians." The Catholic Register, 6 March, 2015 (Accessed
2015-03-10).
20. Weatherbe S.
"Doctors who oppose abortion should leave family medicine: Ontario College
of Physicians." LifeSite News, 19 December, 2014 (Accessed
2015-02-26).
21. College of Physicians and Surgeons of
Ontario, About the College:
Self Regulation and the Practice of Medicine (Accessed 2015-03-22)
Prev | Next