Good News and Bad News
Presentation to the Catholic Physicians' Guild of Vancouver
North
Vancouver B.C. (22 November, 2014)
Full Text

Introduction
Thank you for inviting me to speak this evening. I have never been asked
to give a three hour presentation to a group of physicians. You will be
relieved to know that I have not been asked to do that tonight.
Those of you who saw the BC Catholic headline may have been expecting a
"lecture on medical ethics," but, thanks to Dr. Bright's introduction, you
now know that I am an administrator, not an ethicist, and that my topic is
freedom of conscience in health care.
Protection of Conscience Project
The Protection of Conscience Project will be 15 years old this December.
Although a meeting sponsored by the Catholic Physicians Guild provided the
impetus for its formation, the Project is a non-denominational initiative,
not a Catholic enterprise. Thus, if I mention the Catholic Church or
Catholic teaching tonight, it will be as an outsider, as it were, though an
outsider with inside information.
One more thing: the Project does not take a position on the acceptability
of morally contested procedures like abortion, contraception or euthanasia:
not even on torture. The focus is exclusively on freedom of conscience.
Context
 The context for my presentation is provided by the passage of the Quebec
euthanasia law1 and the pending decision in Carter
v. Canada in the
Supreme Court.2 Physicians are now confronted by the
prospect that laws against euthanasia and physician assisted suicide will be
struck down or changed. If that happens, what does the future hold for
Catholic physicians and others who share your beliefs?
The context for my presentation is provided by the passage of the Quebec
euthanasia law1 and the pending decision in Carter
v. Canada in the
Supreme Court.2 Physicians are now confronted by the
prospect that laws against euthanasia and physician assisted suicide will be
struck down or changed. If that happens, what does the future hold for
Catholic physicians and others who share your beliefs?
Will you be forced to participate in suicide or euthanasia?
If you refuse, will you be disadvantaged, discriminated against,
disciplined, sued or fired?
Will you be forced out of your specialty or
profession, or forced to emigrate if you wish to continue in it?
What about those who come after you? If you avoid all of these
difficulties, will they?
In sum, will freedom of conscience and religion
for health care workers be protected if assisted suicide and euthanasia are
legalized?
These questions and the issues and problems they raise have been largely
avoided or glossed over.
They have been avoided by opponents of assisted suicide and
euthanasia because, understandably, they don't want to compromise their
central message: don't do it.
They have been glossed over by advocates of assisted suicide and
euthanasia because they are afraid that support for legalization may
evaporate if people think that unwilling physicians will be forced to kill
patients. Instead, they adopt a reassuring posture of respect for freedom of
conscience and tolerance for opposing views.
I will suggest tonight that we have reached the point at which these
questions and the problems they bring with them can no longer be avoided,
nor can they be glossed over with saccharine promises of respect and
tolerance.
Carter v. Canada
The common law that came to Canada from England recognized that suicide
can be deliberately chosen by someone who is of sound mind, but viewed such
acts as always immoral and contrary to reason.3 Deliberate choice was
understood to make suicide more wrongful, not less. Consistent with this
tradition, many people - Catholic physicians among them - continue to
believe that suicide, while not blameworthy if it results from mental or
emotional disorder, is immoral or unethical if deliberately chosen, should
always be prevented, and should never, ever be encouraged or assisted.
 However, the ruling of Madame Justice Smith in Carter v. Canada
was based on a radically different fundamental premise. She held that
suicide is not always wrong: that it can, in some circumstances, be a
rational and moral act.4 In other words, she believed that it can sometimes
be a good thing to commit suicide. Logically, if it is good to commit
suicide in some circumstances, it must, in those circumstances, be good to
assist with suicide.5
However, the ruling of Madame Justice Smith in Carter v. Canada
was based on a radically different fundamental premise. She held that
suicide is not always wrong: that it can, in some circumstances, be a
rational and moral act.4 In other words, she believed that it can sometimes
be a good thing to commit suicide. Logically, if it is good to commit
suicide in some circumstances, it must, in those circumstances, be good to
assist with suicide.5
Granted this, it must also be a good thing, in those circumstances, to do
for someone like Gloria Taylor what she wants to do but is unable to do: to
end her life - to kill her. Thus, the judge's reasoning moved logically from
approving suicide, to approving assisted suicide, and then to approving
euthanasia.
According to Madame Justice Smith, the purpose of the law is not to
prevent all suicides or all assisted suicides. The sole purpose of the law
is to protect vulnerable people, who, in moments of weakness, might be
tempted to kill themselves without sufficient reason and reflection.6 Having
established this, she framed the key questions.
Can vulnerable people be adequately protected only by the absolute
prohibition of assisted suicide?
Or is there a less drastic alternative that can achieve the same goal?
The burden was on the defendant governments to prove that vulnerable
people cannot not be protected by anything less than absolute prohibition.7
They produced evidence of risk, which the judge accepted.8 However, the
effect of this evidence was significantly diminished because the judge
defined the goal as one of managing or reducing risk - not eliminating it
altogether.9 She concluded that the risks could be reduced to acceptable
levels.10
I suggest that her belief that suicide could sometimes be a good thing
led her to adopt the policy of risk management. I suggest she would not have
been so inclined in the case of something she believed to be always gravely
immoral. For example, if the subject were sexual assault, I doubt that she
would recommend risk reduction rather than risk elimination. I don't think
she would attempt to calculate an acceptable level of risk for rape.
For these reasons, I suggest that the trial court ruling in Carter hinged
entirely upon the foundational premise that killing oneself can sometimes be
a good thing. The premise was not challenged during the trial. Instead, the
defence of the law depended largely upon utilitarian arguments about the
ineffectiveness of safeguards, the risks to vulnerable people and slippery
slopes.
Now, I don't mean to denigrate those who did their best to defend the
law. In the first place, I am tackling this from a different perspective.
Moreover, the defendant governments probably believed - with good reason -
that moral arguments would be abruptly dismissed, with contempt or
condescension. However, keeping silent about morality does not produce a
morally neutral judicial forum. It simply allows the judge's moral beliefs
to set the parameters for argument and adjudication.
This applies not only in courtrooms, but in the public square.
 This was illustrated during CBC's Cross Country Checkup following the
Carter decision.11 Most of those who opposed the ruling argued, as the
defendant governments did at trial, that assisted suicide and euthanasia
should not be legalized because that would endanger vulnerable people.
This was illustrated during CBC's Cross Country Checkup following the
Carter decision.11 Most of those who opposed the ruling argued, as the
defendant governments did at trial, that assisted suicide and euthanasia
should not be legalized because that would endanger vulnerable people.
But when asked if they would deprive Gloria Taylor of the right to
physician-assisted suicide, every one of them avoided the question. Not one
said that she should be denied help to kill herself.
They had argued against legalizing assisted suicide solely because of the
risk that vulnerable people would be exploited, and no safeguards could
adequately protect them. But Gloria Taylor could not plausibly be described
as a vulnerable and exploited person in need of protection, so they could
not explain why, in her case, assisted suicide should not be permitted.
And if they could offer no reason to deny it to her, upon what basis
would they deny it to others similarly situated? And what reason would they
have to refuse to help her kill herself?
Had they argued from the outset
against suicide and euthanasia on moral, philosophical or religious grounds
(though not excluding others), they might have been able to answer
differently. But, like the government defendants, they did not do so, and
were placed in a very awkward spot by the interviewer.
As you might be by a patient if the law is changed. In the case of
conscientious objection, silence about one's moral, religious or
philosophical beliefs is impossible.
Rights claims
Once suicide, assisted
suicide and euthanasia are understood to be benefits, it is possible to
assert that one has a right to them, at least in defined circumstances. The
Quebec euthanasia law purports to enact such a right,12 and the BC Civil
Liberties Association and others claim such a right in Carter.13 Such claims
imply that, in some circumstances, physicians have a legal or professional
obligation to kill a patient or to help a patient kill himself.
A statement by new CMA President, Dr. Chris Simpson, can be understood to
support that view. Responding to a suggestion that someone other than
physicians should provide euthanasia and assisted suicide, he said, "I don't
think we want to be reneging on our responsibilities to serve our patients."14
That is the language of obligation.
The obligation to kill
I want to dwell for a moment on the obligation to kill, but I should
first clarify my use of the term. I use "killing" in the sense explained by
Beauchamp and Childress in the Principles of Biomedical Ethics:
The term killing does not necessarily entail a
wrongful act or a crime, and the rule
'Do not kill' is not an absolute rule.
Standard justifications of killing, such as killing in self-defense, killing
to rescue a person endangered by another persons' wrongful acts, and killing
by misadventure. . . prevent us from prejudging an action as wrong merely
because it is killing.15
With that out of the way, I want to focus on the obligation to kill
because I don't think the nature of the obligation is sufficiently
appreciated. An obligation to kill must be distinguished from an
authorization to kill or a justification of killing.
 Soldiers and police are legally authorized to kill, and all of us may be
legally justified in killing in self-defence. But neither the authority to
kill nor legal justifications for killing amount to an obligation to kill.
If the first shot merely wounds a bank robber, a policeman is not entitled
to administer a coup-de-grâce. There is no obligation to kill even in
military combat; deliberately killing disabled enemies is a crime.16
Soldiers and police are legally authorized to kill, and all of us may be
legally justified in killing in self-defence. But neither the authority to
kill nor legal justifications for killing amount to an obligation to kill.
If the first shot merely wounds a bank robber, a policeman is not entitled
to administer a coup-de-grâce. There is no obligation to kill even in
military combat; deliberately killing disabled enemies is a crime.16
Once we realize that an obligation to kill is not imposed even upon
people whose duties may entail killing, we can recognize that imposing an
obligation to kill upon physicians would be unique and extraordinary.
But it is not unprecedented.
An obligation to kill was formerly imposed on public executioners. The
essence of that obligation was captured by Blackstone's explanation that
"if, upon judgment to be hanged by the neck till he is dead, the criminal be
not thoroughly killed, but revives, the sheriff must hang him again."17
That is what an obligation to kill would require of a physician. If a
lethal injection failed to kill a patient, a physician would have to inject
the patient again to ensure that he is "thoroughly killed." This is implied
in the Quebec euthanasia law, which requires a physician who administers a
lethal substance to remain with the patient "until death ensues."18
It would thus seem to be difficult to legalize physician-assisted suicide
without also legalizing euthanasia.
Let's suppose a patient seeks assisted suicide to avoid being
incapacitated by a progressive illness. A physician provides the lethal
drug. The patient takes it, but doesn't die. Instead, the drug causes
precisely the kind of incapacitation that the patient wanted to avoid. It
could be argued that the physician who contracted to help the patient kill
himself is obliged to fulfil the terms of the contract: to make sure that a
patient who survives assisted suicide is "thoroughly killed" by euthanasia.
It seems likely that euthanasia will be wanted at least as a backup for
failed assisted suicide, as abortion is wanted as a backup for failed
contraception.19
Good news
Now, my reference to public executioners may be thought inappropriate.
I'll grant that it may cause discomfort, but I think it is instructive with
respect to the nature of the obligation to kill. But Catholic physicians and
others who share your beliefs are looking for assurance that they will not
be expected to kill patients if the Supreme Court strikes down the law. On
this point, there is good news and bad news.
The good news begins with some statistics. These are only approximations,
but they will do for present purposes. (See
Appendix "A")
Belgium
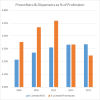
 Euthanasia has been legal in Belgium since 2002, but the number of
physicians directly involved is quite low: I estimate a maximum of 0.62% to
2.3% of all Belgian doctors. The actual number of physicians directly
involved could be much lower. For example, one physician killed 28 patients
in about ten years, which, in official statistics, would be reflected as the
work of 28 physicians, not one.
Euthanasia has been legal in Belgium since 2002, but the number of
physicians directly involved is quite low: I estimate a maximum of 0.62% to
2.3% of all Belgian doctors. The actual number of physicians directly
involved could be much lower. For example, one physician killed 28 patients
in about ten years, which, in official statistics, would be reflected as the
work of 28 physicians, not one.
Netherlands
 In the Netherlands, physicians may provide both euthanasia and assisted
suicide. Dutch General practitioners are the main providers: over 28% of
GP's were directly involved in 2011. But, of all Dutch physicians, it seems
that a maximum of 9% to 12% have been directly involved in reported
euthanasia.
In the Netherlands, physicians may provide both euthanasia and assisted
suicide. Dutch General practitioners are the main providers: over 28% of
GP's were directly involved in 2011. But, of all Dutch physicians, it seems
that a maximum of 9% to 12% have been directly involved in reported
euthanasia.
Taking the opposite view, this indicates that over 80% of Dutch GP's and
88% to 98% of Belgian and Dutch physicians overall are not directly involved
in killing patients. This estimate seems so high as to be improbable, until
we look at the numbers from Oregon and Washington.
Oregon and Washington
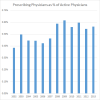 In Oregon, where assisted suicide has been legal since 1997, between
0.38% to 0.62% of the state's active registered physicians wrote
prescriptions for lethal medication between 2002 and 2013. The state of
Washington legalized assisted suicide in 2009. The number of Washington
physicians prescribing lethal medications has increased steadily since then
: from 0.21% to 0.34% of licensed physicians.
In Oregon, where assisted suicide has been legal since 1997, between
0.38% to 0.62% of the state's active registered physicians wrote
prescriptions for lethal medication between 2002 and 2013. The state of
Washington legalized assisted suicide in 2009. The number of Washington
physicians prescribing lethal medications has increased steadily since then
: from 0.21% to 0.34% of licensed physicians.
 I repeat that these are only approximations, but I believe that they
demonstrate that if you refuse to kill patients or assist in consultations
leading to euthanasia or assisted suicide, your practices will reflect the
professional norm. From your perspective, I think that is good news.
I repeat that these are only approximations, but I believe that they
demonstrate that if you refuse to kill patients or assist in consultations
leading to euthanasia or assisted suicide, your practices will reflect the
professional norm. From your perspective, I think that is good news.
We
find more good news by turning once more to Carter and the Quebec euthanasia
law.
Carter v. Canada
In her ruling in Carter, Madame Justice Smith noted that the plaintiffs
did not assert that physicians should be compelled to provide euthanasia or
assist in suicide.21 Lawyer Joseph Arvay opposed the Project's intervention in
the Carter appeal because his clients had never argued that physicians
should be forced to kill patients,22 and, in his oral submission, said, "[N]o
one is suggesting that a physician who has a religious objection to
assisting a patient with his or her death must do so."23
Quebec euthanasia law
Quebec intervened in the Carter appeal to advocate for its euthanasia
law. When asked about the law's protection for conscientious objectors,
Quebec's lawyer said the law "allows a doctor to refuse to administer aid in
dying" and that physicians would "never [be] compelled to act against their
conscience."24 The Quebec Association for the Right to Die with Dignity had
previously assured Quebec legislators that it had no intention of forcing
physicians to provide euthanasia.25
Canadian Medical Association
Finally, the Canadian Medical Association's intervention in Carter
referred to the motion supporting "the right of all physicians. . . to
follow their consciences when deciding whether or not" to provide assisted
suicide or euthanasia.26 The CMA insisted that the law should protect both
physicians providing the procedures and those who do not.27
[N]o physician should be compelled to participate in
or provide medical aid in dying to a patient, either at all, because the
physician conscientiously objects . . . or in individual cases, in which the
physician makes a clinical assessment that the patient's decision is
contrary to the patient's best interests.28
There you have it. If you refuse to kill patients for reasons of
conscience, your refusal be consistent with the practice of an overwhelming
majority of physicians. Moreover, you have the solemn promises of euthanasia
activists and the Quebec government, made publicly before a legislative
committee and the Supreme Court of Canada, that you will never be forced to
do so. Finally, you have the support of the Canadian Medical Association,
underwritten by their intervention in Carter.
There you have the good news.
The bad news
On the one hand, the Quebec government and the plaintiffs in the Carter
case are asking the Supreme Court to declare that patients have a
constitutional right to physician assisted suicide and euthanasia. On the
other, we know that most physicians do not kill their patients or help them
kill themselves.
This has the makings of a first class train wreck.
If the Supreme Court strikes down the law, how can the Quebec government,
Mr. Arvay and the BC Civil Liberties Association ensure that patients will
be able to access euthanasia and assisted suicide without breaking their
promise that objecting physicians will not have to kill patients?
The answer is that they will keep their promises - to the letter.
Mandatory referral implicit in Carter
You will not have to kill. That will not be expected. But you will be
expected to cooperate. If, for reasons of conscience or religion, you won't
kill a patient or help him to kill himself, you will not have to. All you
will have to do is help the patient find someone who will. They promised
that you would not have to kill. They did not promise that you would not
have to find someone else to do it. This has been in the cards from the
beginning. That's why the Project joined the Catholic Civil Rights League
and Faith and Freedom Alliance as an intervener in Carter.
An obligation to at least facilitate euthanasia and assisted suicide was
implicit in Mr. Arvay's factum.29 It was implicit in his notice of claim30 and
in the testimony of his witness, Professor Margaret Battin. She implied that
a physician's refusal to provide assisted suicide or euthanasia
 would amount
to unethical abandonment of patients.31 Mr. Arvay introduced into evidence32 a
report by a Royal Society panel of experts. It stated that if religious or
moral conscience prevents health professionals from killing patients or
assisting in suicide, "they are duty bound to refer their patients to a
health care professional who will."33 One of the authors of the report was
Professor Jocelyn Downie of Dalhousie University. Professor Downie helped
prepare Mr. Arvay's expert witnesses for the trial.34
would amount
to unethical abandonment of patients.31 Mr. Arvay introduced into evidence32 a
report by a Royal Society panel of experts. It stated that if religious or
moral conscience prevents health professionals from killing patients or
assisting in suicide, "they are duty bound to refer their patients to a
health care professional who will."33 One of the authors of the report was
Professor Jocelyn Downie of Dalhousie University. Professor Downie helped
prepare Mr. Arvay's expert witnesses for the trial.34
Mandatory referral implicit in Quebec euthanasia law
An undetermined number of physicians who don't want to kill patients or
assist with suicide may, in fact, be willing to refer patients to colleagues
who will. The Protection of Conscience Project won't hear from them. But
many physicians will not be willing to refer patients because they believe
that helping to arrange a killing makes them a participant in it. This was
very succinctly explained by the President and Director General of Quebec's
Collège des médecins, Dr. Charles Bernard. He said,
[I]f you have a conscientious objection and it is you
who must undertake to find someone who will do it, at this time, your
conscientious objection is [nullified]. It is as if you did it anyway. /
[Original French] Parce que, si on a une objection de conscience puis c'est
nous qui doive faire la démarche pour trouver la personne qui va le faire, à
ce moment-là , notre objection de conscience ne s'applique plus.
C'est comme si on le faisait quand même.35
 This is a striking admission, because it is an indictment of Dr.
Bernard's own Code of Ethics. The Collège des médecins
Code of Ethics
requires that physicians unwilling to provide a service for reasons of
conscience "offer to help the patient find another physician."36
This is a striking admission, because it is an indictment of Dr.
Bernard's own Code of Ethics. The Collège des médecins
Code of Ethics
requires that physicians unwilling to provide a service for reasons of
conscience "offer to help the patient find another physician."36
Quebec's euthanasia law allows physicians to refuse to kill patients, but
adds that they "must nevertheless ensure that continuity of care . . . in
accordance with their code of ethics"37 - and that demands referral.
This is what Quebec's lawyer left out when he told the Supreme Court that
physicians would "never [be] compelled to act against their conscience." The
Project's lawyer drew the contradiction to the attention of the Court, using
it as an example of "precisely the sort of thinking that, in our submission,
ought to be protected against."38
Canadian Medical Association and mandatory referral
Much more could be said on that score, but let's look more closely at the
Canadian Medical Association's intervention. The Association's factum
stated, "[N]o physician should be compelled to participate in or provide"
the services. Surely this means that the CMA will support physicians who
refuse to help patients find someone to kill them.
Not necessarily. The devil is in the footnotes.
The factum states that "no jurisdiction that has legalized medical aid in
dying compels physician participation."39
However, the footnote to this comment includes a citation of the Quebec
euthanasia law, which, as we have just seen, is less than satisfactory. The
factum continues:
If the attending physician declines to participate,
every jurisdiction that has legalized medical aid in dying has adopted a
process for eligible patients to be transferred to a participating
physician.40
 Here the footnote cites an addendum, "Schedule A," part of a package
prepared for the August AGM.41 Schedule A states that objecting physicians in
Washington, Vermont, Oregon, Belgium, and Luxembourg "have a duty to
transfer patient care to another physician who can fulfil the request."42
Here the footnote cites an addendum, "Schedule A," part of a package
prepared for the August AGM.41 Schedule A states that objecting physicians in
Washington, Vermont, Oregon, Belgium, and Luxembourg "have a duty to
transfer patient care to another physician who can fulfil the request."42
This is erroneous, misleading and troubling.
It is erroneous because the law in Vermont says nothing of the sort: in
fact, says nothing at all about this.43
It is misleading because it could be taken to mean that the objecting
physician has a duty to initiate the transfer to a willing colleague. This
is not required in any of the jurisdictions listed. All that is required is
that objecting physicians transfer the patient's medical records as
requested by the patient.44
So, erroneous and misleading.
It is troubling for two reasons
- First: the error and slant in the presentation favours the view that
failure to initiate a referral or transfer for euthanasia constitutes
patient abandonment.
- Second: I have had access to a document that indicates that this is the
view of influential CMA staffers..
I will not be more specific because I do not burn my sources, but I do
not think that sloppy research and clumsy draftsmanship adequately account
for the wording of Schedule A.
More direct evidence is available in the Association's oral submission.
This referred only to the need to avoid "overriding the consciences of those
who object to performing" euthanasia or assisted suicide and to respect "the
choice of those who do not wish to perform the practice."45
These
statements certainly do not engender confidence that the Canadian Medical
Association will support physicians who refuse to help patients find someone
to kill them.
So what did the CMA mean when it said "no physician should be compelled
to participate in or provide" euthanasia or assisted suicide?
I don't know. It all depends upon what the Association means by
"participate." I'm not a member of the CMA, but, if I were, I would make it
my business to find out.
What the future holds
Now, if the Supreme Court strikes down the law, an undetermined number of
physicians and health care workers will eventually begin to kill patients,
in the belief that what they were doing is not only legal, but morally
acceptable. In a sense, this would not be remarkable, because that sort of
thing has happened in the past, and it is happening now, in Belgium, the
Netherlands and Luxembourg, for example.
Nonetheless, many physicians and health care workers will, despite the
ruling, continue to consider euthanasia to be (morally) planned and
deliberate homicide. They will likely refuse to kill patients and refuse to
encourage or facilitate the killing of patients by counselling, referral or
other means.
And then the Collège des médecins du Québec, the Royal Society of Canada,
Professor Downie, and the BC Civil Liberties Association and others will
play the mandatory referral card. They will demand that health care
professionals be compelled to facilitate the killing of patients by referral
and other means.
How can I be sure of this?
Because some of them are already making these demands, and all of them
have been rehearsing this play for years. The last full-scale dress
rehearsal was in Ottawa. Three of your colleagues played starring roles.
Dress rehearsal in Ottawa
 The play opened in January, when a 25 year old woman was unable to get a
prescription for birth control pills at an Ottawa walk-in clinic. The
physician on duty was a Catholic with an NFP only practice. The receptionist
gave the woman a letterexplaining that he did not prescribe or refer for
contraceptives for reasons of "medical judgment as well as professional
ethical concerns and religious values." She obtained the prescription at a
clinic two minutes away.46
The play opened in January, when a 25 year old woman was unable to get a
prescription for birth control pills at an Ottawa walk-in clinic. The
physician on duty was a Catholic with an NFP only practice. The receptionist
gave the woman a letterexplaining that he did not prescribe or refer for
contraceptives for reasons of "medical judgment as well as professional
ethical concerns and religious values." She obtained the prescription at a
clinic two minutes away.46
The physician was not forced to do something
contrary to his medical judgement and religious beliefs, and the young woman
obtained birth control pills by driving around the block. In more tolerant
times and places this might have been considered a successful compromise. In
this case, it sparked a witch hunt. Two more NFP only physicians - both
Catholics - were discovered lurking in the nation's capital.
The
three NFP only physicians account for 0.076% of about 4,000 physicians
practising in the Ottawa area,47 so at least potentially, 99.9% of Ottawa area
physicians are willing to prescribe contraceptives.
Nonetheless, a venomous feeding frenzy erupted on Facebook. News that
three out of 4,000 area physicians did not prescribe The Pill made
headlines.48 It was front page news and a public scandal that three Ottawa
physicians would not recommend, facilitate or do what they believed to be
immoral, unethical, or harmful. Consulted by an Ottawa Citizen columnist,
officials from the CMA and the CPSO seemed unsure about whether or not there
is room for that kind of integrity in the medical profession.49 A few days
later, a reporter with the Medical Post expressed doubt that it was even
legal.50 It eventually became the subject of a province-wide CBC Radio
programme.51
This was a wildly disproportionate response to news that a young woman
had to drive around the block to get birth control pills.
Why do I call this a rehearsal for confrontations about assisted suicide
and euthanasia?
A duty to refer patients to be killed
Because the arguments said to justify compelling objecting physicians to
provide or refer for contraception and abortion are the same arguments used
to try to compel objecting physicians to provide or facilitate euthanasia
and assisted suicide. I won't attempt to cover them tonight, but I will give
you a single example that demonstrates the connection.
In 2006 Jocelyn Downie was one of two law professors who wrote a guest
editorial in the Canadian Medical Association Journal claiming that
physicians who refuse to provide abortions for reasons of conscience had an
ethical and legal obligation to refer patients to someone who
would.52 Five
years later she was a member of the "expert panel" of the Royal Society of
Canada that, as we have seen, recommended that health care professionals who
object to killing patients should be compelled to refer patients to someone
who would.53 The experts argued that, because it is agreed that we can compel
objecting health care professionals to refer for "reproductive health
services," we are justified in forcing them to refer for euthanasia.54
Jocelyn Downie and Daniel Weinstock, another member of the Royal Society
expert panel, are members of the faculty of the "Conscience Research Group."56
This is a quarter-million dollar Canadian Institutes of Health Research
(CIHR) funded project.57 It is headed by Professor Carolyn McLeod and
supported by a research assistant and seven graduate students. A central
goal of the group is to entrench in medical practice a duty to refer for or
otherwise facilitate contraception, abortion and other "reproductive health"
services. From the perspective of many objecting physicians, this amounts to
imposing a duty to do what they believe to be wrong.
But that is just what the Conscience Research Group and others propose:
that the state or a profession can impose upon physicians a duty to do what
they believe to be wrong - even if it is killing someone - even if they
believe it to be murder - and that they should be punished if they refuse.
Killing is not surprising; even murder is not surprising. But to hold
that the state or a profession can, in justice, compel an unwilling soul to
commit or even to facilitate what he sees as murder, and justly punish or
penalize him for refusing to do so - to make that claim is extraordinary,
and extraordinarily dangerous. For if the state or a profession can require
me to kill someone else - even if I am convinced that doing so is murder -
what can it not require?
Conclusion
How can we possibly have arrived at this point?
By first convincing people that contraception is a good thing, and that
physicians should be made to prescribe or refer for contraception.
By then convincing them that abortion is a good thing, and that
physicians should be made to perform or refer for abortion.
Finally, as Madame Justice Smith has demonstrated, by convincing people
that suicide, then assisted suicide, and then euthanasia are good things,
and that physicians should be made to provide or refer for them.
Convince people that X is a good thing - whatever X might be - and the
rest will follow - especially if X offers power, sex or relief from
suffering.
When laws governing abortion and contraception became less restrictive
almost fifty years ago, the kind of attacks now being made on physicians and
other health care workers who decline to provide or facilitate the services
was beyond imagining. No one would then have anticipated that the more
liberal society they thought they were building would generate the
vituperative intolerance now evident in Ontario.
So how can we know what the future holds for Catholic physicians and
others who share your beliefs if the Supreme Court legalizes assisted
suicide and euthanasia?
You might ask your three Ottawa colleagues.
And then you might read G.K. Chesterton's Ballad of the White Horse.
Closing
I again thank you for inviting me to speak tonight.
If my presentation has not been quite what you were expecting, I hope
that you will at least be able to thank Dr. Bright for referring a pleasant
61 year old gentleman to you for consultation.
Notes
1. Bill 52,
An Act respecting end-of-life
care.
(Hereinafter "ARELC.")
2.
Lee Carter, et al. v. Attorney General of
Canada, et al. Supreme Court of Canada, Case 35591
(Accessed 2014-11-24).
3. "The party must be of years of discretion,
and in his senses, else it is no crime. But this excuse ought not to be
strained to that length, to which our coroner’s juries are apt to carry
it, viz. that the very act of suicide is an evidence of insanity; as if
every man, who acts contrary to reason, had no reason at all: for the
same argument would prove every other criminal non compos, as well as
the self-murderer. The law very rationally judges that every melancholy
or hypochondriac fit does not deprive a man of the capacity of
discerning right from wrong; which is necessary, as was observed in a
former chapter, to form a legal excuse." Blackstone, William,
Commentaries on the Laws of England (12th ed), Vol. IV. London: A.
Strahan and W. Woodfall, 1795, p. 188-189.
4.
Carter v. Canada (Attorney General) 2012
BCSC 886. Supreme Court of British Columbia, 15 June, 2012. Vancouver,
British Columbia. (Hereinafter "Carter v. Canada") para. 339
(Accessed 2014-11-24) The qualifications "rationally and
morally"are implicit in the reasoning but not stated. The judge uses the
term "ethical," not "moral," and more frequently employs the former, but
she treats them as synonyms when addressing the question, "Does the law
attempt to uphold a conception of morality inconsistent with the
consensus in Canadian society?" (para. 340-358) Moreover, witnesses on
both sides do not typically distinguish between ethical and moral
issues. See, for example, Dr. Shoichet (plaintiffs) at para. 75, Prof.
Sumner (plaintiffs) at para. 237, Dr. Bereza (defendants) at para. 248,
Dr. Preston (plaintiffs) at para. 262. The judge defines ethics as "a
discipline consisting of rational inquiry into questions of right and
wrong" and frames the question accordingly: " whether it is right, or
wrong, to assist persons who request assistance in ending their lives
and, if it is right to do so, in what circumstances." Carter v. Canada,
para. 164. Most would see in this passage no way to distinguish between
ethics and moral philosophy.
5. Murphy S. "Legalizing therapeutic
homicide and assisted suicide: A tour of Carter v. Canada."-
VI.1-
Finding of "discrimination." Protection of Conscience Project.
6. Carter v. Canada, para. 16, 926,
1116, 1126, 1166, 1184-1185, 1187-1188, 1190, 1199, 1348, 1362
7. Carter v. Canada, para. 1172, 1348
8. For example, Carter v. Canada, para. 653,
815
9. Carter v. Canada, para. 1240
10. Carter v. Canada, para. 1243, 1283
11. CBC Radio,
Cross Country Checkup,
24 June, 2012.
(Accessed 2012-06-28).
12.
Section 4 of ARELC
states that eligible patients have a right to "end-of life-care," which
includes euthanasia and palliative care.
13. In the BCSC,
Amended Notice of Civil
Claim, Part 1, para. 64(c), Part 3, para. 5-7, 9-1; In the SCC on
appeal from the BCCA,
Factum of the Appellants,
para. 4, 123, 162-164, 182(e). (Accessed 2014-10-14)
14. Kirkey S.
"Doctor-assisted death
appropriate only after all other choices exhausted, CMA
president says." canada.com, 26 August, 2014
(Accessed 2014-10-06).
15. Beauchamp TL, Childress JF, Principles
of Biomedical Ethics (7th ed.) New York: Oxford University Press, 2013,
p. 176
16. Moore, O.
"Former Canadian army officer
accused of murder speaks out." Globe and Mail, 4 September, 2012.
(Accessed 2014-08-14).
17. Blackstone, W. Commentaries on the
Laws of England (12th ed.), Vol. 4. London: Strahan & Woodfall, 1795, p.
405. Citing 2 Hal. P.C. 412, 2 Hawk. P.C. 463
18.
ARELC, section 30.
19. Ann Furedi the chief executive of the
British Pregnancy Advisory Service, told New Zealanders that abortion is
required as a part of family planning programmes because contraception
is not always effective. She noted that abortion rates do not drop when
more effective means of contraception are available because women are no
longer willing to tolerate the consequences of contraceptive failure.
Abortion a necessary option: advocate. 18 October, 2010, TVNZ.
(Accessed 2014-02-15). Over twenty years ago, the U.S. Supreme Court
stated that "for two decades of economic and social developments, people
have organized intimate relationships and made choices that define their
views of themselves and their places in society, in reliance on the
availability of abortion in the event that contraception should fail.
The ability of women to participate equally in the economic and social
life of the Nation has been facilitated by their ability to control
their reproductive lives."
Planned Parenthood of Southeastern Pa. v.
Casey - 505 U.S. 833 (1992), p. 856
(Accessed
2014-02-15).
20. Cook Michael,
"First-world problems 2:
I’m really not into the whole 'turbo-euthanasia' thing." Bioedge, 27
June, 2013.
(Accessed 2014-07-15)
21. Carter v. Canada,
para. 311.
22. In the SCC on appeal from the BCCA,
Appellants' Response to Motions to Intervene,
20 June, 2014, para. 5(c)
23. Murphy S.
"Re: Joint intervention in
Carter v. Canada-Selections from oral submissions." Supreme Court of
Canada, 15 October, 2014. Joseph Arvay, Q.C. (Counsel for the
Appellants). Protection of Conscience Project.
24. Murphy S.
"Re: Joint
intervention in Carter v. Canada-Selections from oral submissions." Supreme
Court of Canada, 15 October, 2014. Jean-Yves Bernard (Counsel for the
Attorney General of Quebec) Protection of Conscience Project.
25. Consultations, Wednesday, 25 September
2013 - Vol. 43 no. 38: Quebec Association for the Right to Die with
Dignity (Hélène Bolduc, Dr. Marcel Boisvert, Dr. Georges L'Espérance),
T#107
26. In the SCC on appeal from the BCCA,
Factum of the Intervener, The Canadian Medical Association,
para. 3
27. In the SCC on appeal from the BCCA,
Factum of the Intervener, The Canadian Medical Association,
para. 28
28. In the SCC on appeal from the BCCA,
Factum of the Intervener, The Canadian Medical Association,
para. 27
29. In the SCC on appeal from the BCCA,
Factum of the Appellants
(13 May, 2014) para. 4, 123, 162-164 (Accessed 2014-10-14)
30. In the BCSC,
Amended Notice of Civil
Claim, Part 1, para. 55, 64(c); Part 3, para. 9-11, 18.
31. Carter v. Canada, para. 239-240.
Others have made the same claim: see Angell M., Lowenstein E.
"Letter
re: Redefining Physicians' Role in Assisted Dying." N Engl J Med
2013;
368:485-486 January 31, 2013 DOI: 10.1056/NEJMc1209798 (Accessed
2014-11-25)
32. Carter v. Canada, para. 120-130
33. Schuklenk U, van Delden J.J.M, Downie J,
McLean S, Upshur R, Weinstock D.
Report of the Royal Society of Canada
Expert Panel on End-of-Life Decision Making (November, 2011) p. 70
(Accessed 2014-02-23).
34. Carter v. Canada, para. 124
35. Consultations, Tuesday 17 September
2013 - Vol. 43 no. 34: Collège des médecins du Québec, (Dr. Charles
Bernard, Dr. Yves Robert, Dr. Michelle Marchand)
T#154
36. Collège des médecins du Québec,
Code of
Ethics of Physicians, para. 24
(Accessed
2013-06-23)
37.
ARELC, Section 50.
38. Murphy S. "Re: Joint intervention in
Carter v. Canada-Selections from oral submissions." Supreme Court of
Canada, 15 October, 2014.
Robert W. Staley (Counsel for the Catholic
Civil Rights League, Faith and Freedom Alliance, and Protection of
Conscience Project) Protection of Conscience Project.
39. In the SCC on appeal from the BCCA,
Factum of the Intervener, The Canadian Medical Association,
para. 27
40. In the SCC on appeal from the BCCA,
Factum of the Intervener, The Canadian Medical Association,
para. 27
41. Canadian Medical Association,
Reports to
the General Council. CMA 147th Annual General Meeting, August 17-20,
2014.
(Accessed 2014-11-20)
42. Canadian Medical Association,
Schedule
A: Legal Status of Physician Assisted Death (PAD) in Jurisdictions with
Legislation.
43. Vermont Statutes Title 18: Health,
Chapter 113:
An act relating to patient choice and control at end of
life. (Accessed 2014-11-20).
44. Belgium:
"At the request of the patient or the person taken in confidence, the
physician who refuses to perform euthanasia must communicate the
patient's medical record to the physician designated by the patient or
person taken in confidence."
Luxembourg: "A physician who
refuses to comply with a request for euthanasia or assisted suicide is
required, at the request of the patient or support person, to
communicate the patient's medical record to the doctor appointed by him
or by the support person."
Washington: "If a health
care provider is unable or unwilling to carry out a patient's request
under this chapter, and the patient transfers his or her care to a new
health care provider, the prior health care provider shall transfer,
upon request, a copy of the patient's relevant medical records to the
new health care provider."
Oregon: "If a health care
provider is unable or unwilling to carry out a patient's request under
ORS 127.800 to 127.897, and the patient transfers his or her care to a
new health care provider, the prior health care provider shall transfer,
upon request, a copy of the patient's relevant medical records to the
new health care provider."
45. Murphy S.
"Re: Joint intervention in
Carter v. Canada - Selections from oral submissions." Supreme Court of
Canada, 15 October, 2014. Harry Underwood (Counsel for the Canadian
Medical Association) Protection of Conscience Project.
46. Murphy S.
"NO MORE CHRISTIAN DOCTORS."
Protection of Conscience Project, March, 2014.
47. College of Physicians and Surgeons of
Ontario,
All Doctor Search
(Accessed
2014-07-29)
48. Payne E.
"Some Ottawa doctors refuse to
prescribe birth control pills." Ottawa Citizen, 30 January, 2014
(Accessed 2014-08-03)
49. Payne E.
"Some Ottawa doctors refuse to
prescribe birth control pills." Ottawa Citizen, 30 January, 2014
(Accessed 2014-08-03)
50.
Glauser W. "Ottawa clinic doctors’ refusal to offer contraception
shameful,
says embarrassed patient." Medical Post, 5 February, 2014
51. CBC Radio,
"Should doctors have the
right to say no to prescribing birth control?" Ontario Today, 25
February, 2014
(Accessed 2014-11-25)
52. Rodgers S. Downie J.
"Abortion: Ensuring
Access." CMAJ July 4, 2006 vol. 175 no. 1 doi: 10.1503/cmaj.060548
(Accessed 2014-02-23).
53. Schuklenk U, van Delden J.J.M, Downie
J, McLean S, Upshur R, Weinstock D.
Report of the Royal Society of Canada
Expert Panel on End-of-Life Decision Making (November, 2011) p.
101 (Accessed 2014-02-23)
54. Schuklenk U, van Delden J.J.M, Downie J,
McLean S, Upshur R, Weinstock D.
Report of the Royal Society of Canada
Expert Panel on End-of-Life Decision Making (November, 2011) p. 62
(Accessed 2014-02-23)
55.
Let their conscience be their guide?
Conscientious refusals in reproductive health care.
(Accessed 2014-11-21)
56. Let their conscience be their guide?
Conscientious refusals in reproductive health care.
(Accessed 2014-03-07)
57. Canadian Institutes of Health Research,
Let
Conscience Be Their Guide? Conscientious Refusals in Reproductive Health
Care- Project Information.
(Accessed 2014-11-25)