Submission to the Canadian Medical Association Re: 2018 Revision of the CMA Code of Ethics
Full Text

III. CMA on physician freedom of conscience
1988-2012: from abortion to euthanasia
III.1 In 1988, after the Supreme Court of
Canada struck down all legal restrictions on abortion, the CMA
revisited its policies on the procedure. The protection of
conscience provision in the Code of Ethics remained unchanged, and
the Association stressed that there should be no discrimination
against objecting physicians, "particularly for doctors training in
obstetrics and gynecology, and anesthesia."1
III.2 While this reaffirmed the CMA's
commitment to protect physician freedom of conscience, it does not
appear that the foundation for the commitment was explored or
developed over the next 25 years, even in the face of increasingly
strident claims that ultimately led to a recommendation that
objecting physicians should be forced to refer patients for
euthanasia.2
2012-2014: 'neutrality' and conscience
III.3 This issue suddenly came to the fore in
2012 when a ruling by a British Columbia Supreme Court judge struck
down the prohibition of physician assisted suicide and euthanasia.3
When the CMA Annual General Council convened in August, 2013, an
appeal of the Carter decision was in progress, and a euthanasia bill
had been introduced in the Quebec legislature. Council proceedings
reflected "deep divisions within the medical community."4 The Council
did, however, resolve to support "the right of any physician to
exercise conscientious objection when faced with a request for
medical aid in dying." (DM 5-22)5
III.4 CMA officials spent much of 2014 studying
euthanasia and assisted suicide, and in August presented the General
Council with a resolution affirming CMA support for both physicians
unwilling to participate in the procedures, and those willing to do
so, should they be legalized.6 This was explained by CMA officials as
a commitment to neutrality and support for physician freedom of
conscience.7,
8, 9
III.5 However, when the executive revised the
policy in December, it formally approved physician assisted suicide
and euthanasia as "end of life care" and promised to support patient
access to "the full spectrum" of such care, subject only to the law.
The policy did not exclude minors, the incompetent or the mentally
ill, nor did it indicate that the procedures should be provided only
to the terminally ill or those with uncontrollable pain. It referred
directly only persons suffering from "incurable diseases."10 The
Directors thus formally committed the Association to support
euthanasia and assisted suicide not only for competent adults, but
for any patient group and for any reason approved by the courts or
legislatures.
III.6 From a protection of conscience
perspective, the first practical problem with this was that actual
support for euthanasia and assisted suicide within the medical
profession - to the extent that it had been evaluated at all - was
highly volatile. Roughly contemporaneous optimistic estimates
suggested that 6% to 29% of physicians were willing to provide the
procedures, depending upon the condition of the patient; 63% to 78%
would refuse, again dependent upon the condition of the patient. Of
physicians willing to consider providing the services, the number
dropped by almost 50% in the case of non-terminal illness, and by
almost 80% in the case of purely psychological suffering (i.e., in
the absence of pain).11 The Association's unconditional support for
euthanasia and assisted suicide potentially exposed large number of
physicians to demands that could generate serious conflicts of
conscience.
III.7 The second problem was that the policy
was not neutral.12 By classifying euthanasia and assisted suicide as
"end of life care," the CMA executive effectively made participation
in euthanasia and assisted suicide normative for the medical
profession. Once the Supreme Court of Canada ordered legalization of
the procedures,13 the refusal to provide assisted suicide and
euthanasia in the circumstances set out in Carter became an
exception to professional obligations that had to be justified or
excused. This is why, since Carter, public discourse has largely
centred on whether or under what circumstances physicians and
institutions should be allowed to refuse to provide or participate
in homicide and suicide.
III.8 Certainly, the new policy also stated
that the CMA supported the right of physicians to "follow their
conscience" when deciding whether or not to provide euthanasia, and
that physicians "should not be compelled to participate," a broader
term that could encompass referral. However, it characterized the
protection of conscience provision in the Code of Ethics (2004
paragraph 12) as defending only "physician autonomy," not physician moral
agency and personal integrity. In
addition, it added a qualifying statement: "However, there should be
no undue delay in the provision of end of life care." This could be
(and later was) understood to justify limiting freedom of conscience
for objecting physicians in order to ensure patient access to the
services.
2015: the Carter maelstrom
III.9 Thus, when the Supreme Court ruled in
Carter, the CMA was ready to proceed with implementing euthanasia
and assisted suicide, but it was quite unprepared mount a cogent,
articulate and persuasive defence of physician freedom of
conscience. This disadvantage was compounded when the federal
government did virtually nothing for five months following the
ruling, then called (and lost) an election, and left the CMA other
stakeholders scrambling to develop policies responsive to the Carter
ruling without any direction as to what changes would be made to the
criminal law.
III.10 The result was a policy and regulatory
maelstrom that lasted several months. During this time, CMA
officials, struggling to develop practice standards and guidelines
in response to Carter, were also caught between activists demanding
that physicians be compelled to refer for the procedures, and
physicians and physician groups, galvanized by the Carter ruling,
adamantly opposed to providing or facilitating euthanasia or
assisted suicide. Under the circumstances, it is not surprising that
there was some waffling by CMA officials on the issue of referral.
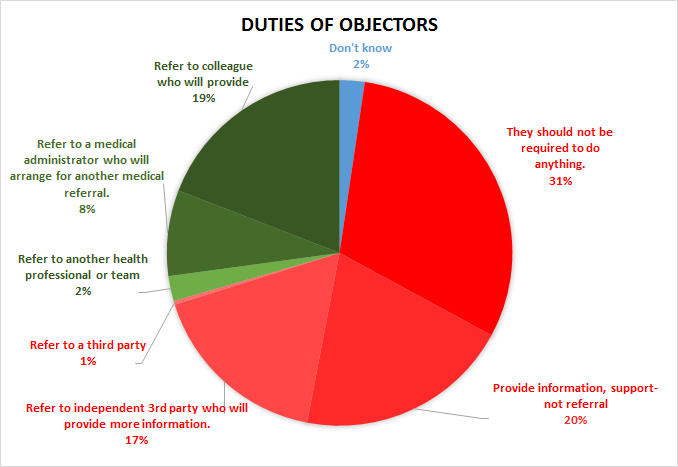
III.11 By the time the Annual General Council
convened in August, 2015, only about 19% of CMA members believed
that physicians should be required to refer patients to someone who
would provide euthanasia or assisted suicide. Almost 70% were
opposed to the idea. About 31% thought objecting physicians should
not be require to do anything, but about 27% believed that they
should provide information and support, or refer to a third party
who
could provide information.
 Source: Murphy S. A
"uniquely Canadian approach" to freedom of conscience in health care: Provincial-Territorial Experts recommend coercion to ensure delivery of euthanasia and assisted suicide. App.
D2.2.3. Protection of Conscience Project (2016).
Source: Murphy S. A
"uniquely Canadian approach" to freedom of conscience in health care: Provincial-Territorial Experts recommend coercion to ensure delivery of euthanasia and assisted suicide. App.
D2.2.3. Protection of Conscience Project (2016).
III.12 The Council ultimately approved a resolution
later adopted by the CMA Board of Directors. It stated that physicians were
not obliged to fulfill requests for or participate in euthanasia or assisted
suicide, and should not be discriminated against for refusing to do so. It
required objecting physicians to provide patients with complete information
on "all options," and advise them "how they can access any separate central
information, counseling, and referral service."14
III.13 This was a development of the basic
framework provided by the Code of Ethics. It was, however, a largely
pragmatic response guided by a general notion of "striking a
balance" between patient and physician autonomy or rights. It was
specific to euthanasia and assisted suicide, and it was unsupported
by principled ethical or philosophical rationale. It is unlikely
that more than this could have been achieved in the circumstances.
2016: The CMA and "effective referral"
III.14 The first CMA statement addressing the
subject of physician freedom of conscience at a foundational level
was a 2016 submission to the College of Physicians and Surgeons of
Ontario in response to its demand that objecting physicians
facilitate euthanasia and assisted suicide by an "effective
referral."15 Important elements of this statement were incorporated
into the new CMA Medical Assistance in Dying policy and are evident
in the 2018 revised draft of the CMA Code of Ethics.
III.15 The first and most important element is
the recognition of physicians as moral agents.
It is in fact in a
patient's best interests and in the public interest for physicians
to act as moral agents, and not as technicians or service providers
devoid of moral judgement. At a time when some feel that we are
seeing increasingly problematic behaviours, and what some view as a
crisis in professionalism, medical regulators ought to be
articulating obligations that encourage moral agency, instead of
imposing a duty that is essentially punitive to those for whom it is
intended and renders an impoverished understanding of conscience.
III.16 The statement does not neglect the
interests of patients seeking access to euthanasia and assisted
suicide, noting that the CMA wishes to protect physician freedom of
conscience "without in any way impeding or delaying patient access."
However, it insists that this can be accomplished by adopting a
two-pronged strategy: by asking physicians to fulfil "a duty that is
widely morally acceptable," yet allows them " to act as moral
agents," and by requiring the community to accept its responsibility
to ensure access, "rather than placing the burden of finding
services solely on individual physicians."
III.17 The third significant point is recognition that the
central concern of objecting physicians is their individual moral
responsibility to avoid complicity in perceived wrongdoing. This is
sometimes misconstrued or misrepresented as a desire to control the
conduct of their patients, and it is too often passed over because
it can be a painful reminder of the essential point of disagreement
between objecting physicians and non-objecting colleagues.
III.18 Fourth, the statement recognizes that
the exercise of freedom of conscience is a fundamental freedom for
everyone, not just for those whose moral judgement conforms to a
dominant viewpoint, or to one's own. This is implied in its
discussion of effective referral. Some physicians who refuse to
provide assisted suicide or euthanasia have no objection to
referring a patient to a colleague willing to provide the service.
Others find referral "categorically morally unacceptable" because
they believe that referral makes them complicit in grave wrongdoing.
The statement characterizes a demand for "effective referral" as
illicit discrimination, not a solution, because it "respects the
conscience of some, but not others."
It is the CMA's strongly
held position that there is no legitimate justification to respect
one notion of conscience . . . the CMA [seeks] to articulate a duty
that achieves an ethical balance between conscientious objection and
patient access in a way that respects differences of conscience. It
is the CMA's position that the only way to authentically respect
conscience is to respect differences of conscience.
III.19 Finally, citing the Supreme Court of
Canada, the statement also emphasizes the fiduciary nature of the
patient-physician relationship: the physician's obligation "to
protect and further their patients' best interests." However, it
adds that physicians' fiduciary obligations do not "in any way"
entail an obligation to violate their own moral integrity.
III.20 The Project has strongly supported this
position for years. However, something more must be added to this.
The dominant view is that "the interests" or "best
interests" of patients are determined by the patients themselves -
not by physicians - even if physicians assist them in deciding what
those interests are. Once patients have identified their interests,
the argument goes, physicians have a fiduciary duty to serve those
interests, by, for example, referring a patient for a desired
procedure. This is erroneous.
III.21 Granted that patients are entitled
to determine what they believe to be in their best interests,
physicians who disagree have no obligation to serve those interests.
As a matter of law, a fiduciary is not a servant.16 Fiduciaries have a
duty not to act under dictation, even the dictation of a
beneficiary,17 and must exercise their own judgement.18 The law does not
allow beneficiaries (patients) to turn fiduciaries (physicians) into
"puppets."19 These are important legal principles that apply to all
aspects of clinical and professional judgement, not just to the
exercise of freedom of conscience.
Conclusion
III.22 The CMA’s support for physician freedom
of conscience has been expressed by resolutions at successive
General Councils. In addition, available statistics indicate that
the great majority of CMA members have been opposed to compelling
objecting physicians to refer for morally contested services, but
seem to agree that there is an obligation to provide information and
to help patients contact other physicians or health care providers.
III.23 Like the 2018 Revision, the CMA's first
statement addressing physician freedom of conscience at a
foundational level emphasizes physician moral agency and integrity.
However, it strongly denounces the imposition of effective referral,
describing it as illicitly discriminatory. This ought to preclude
acceptance of the proposal for referral and physician-initiated
transfer of care in the current text of 2018 Revision C3.
Notes
1. Canadian Medical Association. Policy:
Induced abortion. [Internet] 1988 Dec 15 [cited 2018 Mar 15].
2. Schuklenk U, van Delden JJM, Downie J,
McLean S, Upshur R, Weinstock D.
Report of the Royal Society of Canada Expert Panel on End-of-Life
Decision Making. [Internet] Royal Society of Canada. 2011 Nov.
117 p. [cited 2018 Mar 25] at 69, 101.
3.
Carter v. Canada (Attorney General) 2012 BCSC 886
[Internet] [cited 2018 Mar 15].
4. Eggertson L.
CMA delegates
defer call for national discussion of medically assisted death. CMAJ
[Internet] 2013 Sep 17 [cited 2018 Mar 15];185(13): E623-624.
5. Canadian Medical Association.
Resolutions Adopted,146th Annual Meeting of the Canadian Medical
Association (Calgary, AB) [Internet]. 2013 Aug 19-21 [cited 2022 Oct 8].
6. Canadian Medical Association. 147th
General Council Delegates' Motions [Internet].
End-of-Life Care: Motion DM 5-6 [cited 2022 Oct 8].
7. Kirkey S. Canadian doctors seek freedom to choose whether to offer medical aid in dying. Montreal Gazette [Internet] 2014 Aug 20 [cited 2022 Oct08].
8. Swan M.
Medical association vows to protect conscience rights. The
Catholic Register [Internet]. 2014 Aug 27 [cited 2018 Mar 15].
9. McFadden J.
Yk docs
bring motions on doctor-assisted death: Canadian law on euthanasia could
be overturned by next month. Northern News Services [Internet]. 2014
Sep 8 [cited 2018 Mar 29].
10. Canadian Medical Association. Policy:
Euthanasia and Assisted Death [Internet]. Update 2014 [cited 2022 Oct 08].
11. Murphy S. A "uniquely Canadian approach" to
freedom of conscience: Provincial-Territorial Experts recommend coercion
to ensure delivery of euthanasia and assisted suicide." Appendix "D":
Canadian Medical Association on euthanasia and assisted suicide.
D2.1:
Surveys on support for euthanasia/assisted suicide.
12. Contrast the position of the CMA with
that of the Royal New Zealand College of General
Practitioners, which explicitly declined to endorse euthanasia or
assisted suicide, while recognizing that individual practitioners might
participate if they wished to do so. The Royal New Zealand College
of General Practitioners.
Submission to the Justice Committee re: End of Life Choice Bill
[Internet]. 2018 Mar 6 [cited 2022 Oct 08].
13.
Carter v. Canada (Attorney General), 2015 SCC 5 [Internet]
[cited 2018 Mar 14].
14. Canadian Medical Association.
Principles-based Recommendations for a Canadian Approach to Assisted
Dying. In: CMA Submission to the Federal External Panel on Options
for a Legislative Response to Carter vs. Canada (Federal External Panel)
[Internet]. 2015 Oct 19
[cited 2022 Oct 08]. A2-1 to A2-6 at A2-1,
Foundational Principle 2.
15. Canadian Medical Association.
Submission to the College of Physicians and Surgeons of Ontario:
Consultation on CPSO Interim Guidance on Physician-Assisted Death.
[Internet] 2016 Jan 13.
16.
Canadian Aero Service Ltd. v.
O'Malley, [1974] SCR 592, 1973 CanLII 23 (SCC)
[Internet][cited 2018 Mar 29] ("their
positions . . .charged them with initiatives and with
responsibilities far removed from the obedient role of servants. It
follows that O'Malley and Zarzycki stood in a fiduciary relationship
to Canaero . . ." at 606).
17. United Kingdom, Law Commission, Report
No. 350.
Fiduciary Duties of Investment Intermediaries. Williams Lea
Group for HM Stationery Office. [Internet] 2014 [cited 2022 Oct 08] at para 3.53, note 107, citing
Selby v Bowie (1863) 8 LT 372; Re Brockbank [1948] Ch 206.
18. Ibid, notes 109–110, citing
Thomas G. Thomas on Powers. 2nd ed. Oxford: Oxford University Press;
2012, at para 10.60; Finn P. Fiduciary Obligations. 1st ed. Sydney: Law
Book Co; 1977, at para 44; Mowbray J et al. Lewin on Trusts. 18th ed.
London: Sweet & Maxwell; 2007, at para 29-89.
19. Ibid, para 3.51 note 105,
quoting Finn P. supra note 18 at para 42.
Prev | Next