A "uniquely Canadian approach" to freedom of conscience
Provincial-Territorial Experts recommend coercion to
ensure delivery of euthanasia and assisted suicide
Appendix "D"
Canadian Medical Association on euthanasia and assisted suicide
Full Text

D1. CMA policy: Euthanasia and Assisted Death
(2014)
D1.1 The policy of the Canadian Medical Association (CMA)
on euthanasia and physician assisted suicide (which the CMA calls "assisted
death") does not exclude minors, the
incompetent or the mentally ill, and the policy is not meant to apply only
to the terminally ill or those with uncontrollable pain. It refers directly
only to "patients" and "the suffering of persons with incurable diseases."
The policy, which predates the Carter ruling, classifies euthanasia
and assisted suicide as "end of life care." Under this rubric, the CMA
supports patient access to euthanasia and assisted suicide for any patient
group for any reason and under any circumstances approved by the courts or
legislatures.1
D1.2 By formally approving physician assisted suicide and
euthanasia under circumstances defined by law, the Association has taken the
position that, in those circumstances, physicians have a professional
obligation to kill patients or to help them kill themselves.2 By describing
this as "end of life care," the CMA has made homicide and suicide normative
for the medical profession. It is the refusal to kill patients or assist in
suicide in the circumstances set out in Carter that must be justified or
excused as an exception to professional obligations.
D1.3 Thus, the CMA is prepared to support the exercise of
freedom of conscience and religion by objecting physicians only to the
extent that this does not compromise patient access to euthanasia and
assisted suicide. However, it sets no limits on what non-objecting
physicians might agree to do beyond what might be set by law.
Notwithstanding claims that the Association supports both physicians willing
to provide euthanasia and assisted suicide and those who do not, the
weight and influence of the entire Association has been set against
physicians who believe that it is wrong to kill patients or help them to
kill themselves, or, at least, that physicians should not do so.
D1.4 The formal support of the CMA for
a euthanasia/assisted suicide regime even broader than that proposed in
Carter appears to be in tension with the opinions of many CMA members,
not just objecting physicians. Unlike the Experts, Canadian physicians
are anything but unanimous in their
opinions about euthanasia and physician assisted suicide, and support for
the Carter decision among them is hardly unqualified. This has been
obscured by a habit of presenting the most optimistic view of physician support for
the procedures.
D1.5 Both the habitually optimistic approach and the
volatile nature of the opinions of physicians were evident in the analysis
of CMA surveys offered to delegates at the Annual General Council
(AGC) in August, 2015.
D2. CMA Annual General Council, 2015
D2.1 Surveys on support for
euthanasia/assisted suicide
D2.1.1 A report prepared by CMA officials stated that
"recent polls show that CMA members are evenly divided on the issue of
legalizing assisted dying, and a significant minority of respondents to
these polls said they will participate in offering this service to their
patients."3 The report referred to an
on-line dialogue in which 595 CMA members (less than 1% of the CMA's 80,000
members) "registered to participate."4
It did not acknowledge that only about 150 physicians contributed comments
to the dialogue.
D2.1.2 The details were provided in a presentation by Dr. Jeff Blackmer
at the AGC. Most of his presentation drew from two on-line surveys of about
1.75% and .465% of the CMA membership.
D2.1.3 Using slides, he produced what he called "the key
on-line survey results" of a poll taken after the Carter ruling.
The 2015 survey to which he referred appears to be the on-line survey
consultation survey completed by 1,407 physicians.5 The question asked was,
"Following the Supreme Court of Canada decision regarding medical aid in
dying, would you consider providing medical aid in dying if it was requested
by a patient?"6
D2.1.4 The survey question did not distinguish between
assisted suicide or euthanasia, so we do not know if the respondents
believed that they were answering a question about euthanasia, assisted
suicide or both.
D2.1.5 From the very first, reports about the Carter
decision in the major media constantly and almost uniformly described the
decision as legalizing physician assisted suicide, with no reference to
euthanasia. Dr. Blackmer himself, two weeks after the ruling, claimed that
he was uncertain whether the Court legalized only physician assisted
suicide, or euthanasia as well.7
D2.1.6 Since significantly fewer physicians are willing to
provide euthanasia than assisted suicide,8 the failure to distinguish between
them introduces some uncertainty into the interpretation of the results.
D2.1.7 Note that the survey asked only if physicians would
"consider" providing the procedures, not if they would actually do so.
D2.1.8 29% of those surveyed stated that they would
"consider" it. "That might seem to be a very small percentage," Dr. Blackmer
said, "but when you think of it in terms of absolute numbers, we're talking
tens of thousands of Canadian physicians that are now saying, 'I will
participate.'"9
D2.1.9 Here we see the habitual optimism noted above (D1.4).
In fact, the respondents stated that they would "consider" participating,
not that they would participate. Further, while "tens of thousands" was
arithmetically accurate (29% of 80,000 = 23,200 physicians = 2 x 10,000), the rhetorical slant was toward an optimistic evaluation of the
returns.
D2.1.10 Continuing to 'unpack' the survey results, Dr.
Blackmer told delegates that, of the physicians willing to consider
providing either euthanasia or assisted suicide, "only 20% said yes" with
respect to "someone whose suffering was purely psychological." The actual
number noted in the chart on the slide was 19%, not 20%. He acknowledged
that the response from this statistical subset represented about 6% of the
total number of respondents.10
D2.1.11 "And when we asked, 'Would you provide medical aid
in dying to someone who is not suffering from a terminal illness,' he said,
'43% said yes.'"11
D2.1.12 Dr. Blackmer did not draw attention to the fact that
this appears to represent only about 14% of the total number of respondents.
His slides illustrated the responses proportionate to the subset, not to the
total number of respondents, so the graphic images reflected proportionately
greater support for euthanasia and assisted suicide among respondents (19%
vs. 6%; 43% vs. 14%).
D2.1.13 The slides in the video below draw on the same data
used by Dr. Blackmer in the preceding slides, but graphically represent the
increasingly adverse responses to the conditions specified by the survey
questions.
D2.1.14 An alternative and arguably more useful rendering of
the 2015 survey results is possible.12
● The number of physicians willing to provide euthanasia or assisted suicide
appears to range from 6% to 29%, depending upon the condition of the
patient, and excluding consideration of safeguards.
● The number of physicians unwilling to provide euthanasia or assisted
suicide ranges from 63% to 78%, again depending upon the condition of the
patient, and excluding consideration of safeguards.
● Of physicians willing to consider providing euthanasia or assisted
suicide, the number willing to provide the procedures for non-terminal
illness drops by almost 50% , and drops by almost 80% in the case of purely
psychological suffering (i.e., in the absence of pain), excluding
consideration of safeguards.
D2.1.15 Dr. Blackmer presented a much more optimistic view.
He showed delegates a slide with pie
charts side by side for the purpose of comparing surveys done in 2014,
before the Carter ruling, and in 2015, after it. Delegates
had 24 seconds to take in the following charts and his commentary before he
moved to the next slide.
Blackmer:
So this is before the court decision and after the court decision. And you
can see that the number of participants who said that they were very likely
or likely to participate in assisted dying has actually gone up, from 24% to
29% since the Supreme Court decision.13
D2.1.16 He did not point out that the number of physicians
unwilling to consider providing the service also went up by 5% after the Carter ruling,
from 58% to 63%.
D2.1.17 Again, the survey question asked physicians if they
would consider providing the services, but Dr. Blackmer presented
the responses as indicative of the number of physicians actually willing to
do so.
D2.1.18 Apparently to reinforce the message he wanted to get
across, Dr. Blackmer introduced slides to present data from a survey of
family physicians concerning the Carter decision.14 He cautioned
delegates that "the numbers are a little smaller."15 A "little smaller" seems
to minimize the difference: 372 members compared to 1,407.
D2.1.19 In any case, Dr. Blackmer told delegates that "59% of
members actually said, 'Yes, I agree with that,' so over half of physicians
agreed with the Supreme Court decision."16
Blackmer:
And when they asked, "Would you help a competent, consenting patient end his
or her life," a total of 66% actually said "yes," although most of those -
54% - said, "Yes, but only if appropriate and rigorous checks and balances
are in place.17
D2.1.20 Assuming both slides drew from 372 responses, more
physicians agreed with the Carter decision than were willing to
provide assisted suicide and euthanasia. 27% disagreed with the decision,
but 33% said they would "never" help patients end their lives.
D2.1.21 On the other hand, willingness to
provide euthanasia or assisted suicide was conditional. As Dr. Blackmer
noted, 66% were willing to do so, but the number dropped to 12% in the
absence of "appropriate rigorous checks and balances."
D2.1.22 Most important, Dr. Blackmer left out one critical
word. The actual question (as stated on the slide) was, "Would you help a
competent, consenting DYING patient end his or her life." (Emphasis added)
D2.1.23 The CMA's larger
survey demonstrated that support for euthanasia and assisted suicide among
physicians willing to provide it can drop by almost 50% if the patient is
not terminally ill (D2.1.12-D2.13).
The slide was displayed for only about 15 seconds, so it is doubtful that
many delegates had a chance to reflect on the fact that the survey asked
only about dying patients.
D2.1.24 An alternative and more cautious account of the
College of Family Physicians survey results is possible.
-
Since the Carter decision legalized euthanasia and assisted
suicide for patients who are neither dying nor terminally ill, the value of
the survey in the post-Carter medico-legal landscape is doubtful.
-
In the absence of "appropriate rigorous checks and balances," the number
of family physicians willing to provide euthanasia or assisted suicide drops to only 12% of the total number of respondents.
D2.1.25 Taking time to look at the numbers just as they were
presented,
they did not support the claim that
physicians were "evenly divided" in their opinions about euthanasia and
assisted suicide. The returns indicated that the great
majority of physicians were opposed to both.
Moreover, support for the procedures among favourably disposed physicians
was
highly volatile, depending heavily upon the diagnosis, the condition of the
patient and the rigour of the regulatory regime.
D2.1.26 This was reflected in the Globe and Mail
headline: "Less than a third of doctors willing to aid in assisted dying."18
The National Post response was similar: "Majority of doctors
opposed to participating in assisted death of patients."19 The Canadian
Medical Association Journal acknowledged that "Many doctors won't
provide assisted dying."20
D2.2 Physician freedom of conscience
D2.2.1 Dr. Blackmer introduced what he described as "the
very complex and difficult issue of conscientious objection" with the
results of the on-line survey.21 With respect to the question of what a
physician who refuses to provide euthanasia or assisted suicide should be
required do, "the most popular response" (29%) was, "They should not be
required to do anything."
D2.2.2 25% of the responses were categorized as "other"; this was
unexplained at the General Council.22 The
CMA kindly provided the Project with the summary of the returns
under the category "Other," broken down as follows:
Q4_Other (Please specify). 341 relevant comments, grouped by theme:
|
Provide information and support, but not
referral
|
283 comments
83.0%
|
|
Refer to another health professional or team of
professionals
|
33 comments
9.7%
|
|
Not required to do anything
|
20 comments
5.9%
-
2 comments from respondents who WOULD
consider providing medical aid in dying if it was requested
by a patient
-
18 comments from respondents who would NOT
consider providing medical aid in dying if it was requested
by a patient
|
|
Refer to a third party
|
5 comments
1.5%
|
D2.2.3 When joined to the information that was disclosed at
the Annual General Council (approximated in the Project chart below), it
appears that the great majority of respondents (about 68%) clearly believed
that objecting physicians should not
be required to refer patients for anything other than information.
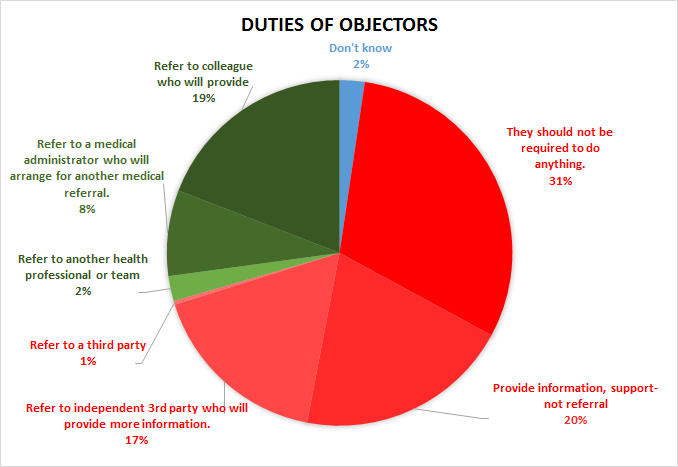
Protection of Conscience Project Chart
D2.2.4 "Effective referral" was favoured by 19% of
respondents, 10% less than the number of physicians who identified
themselves as willing to consider providing euthanasia or assisted suicide
(D2.1.3).
D2.2.5 Returning to the subject later in his presentation,
Dr. Blackmer noted that "the vast majority expressed the view that physician
conscience rights must be integrally protected." He reminded delegates of
the resolution passed at the 2013 Annual ' Council "saying that no
physician should be forced to participate in an assisted dying against their
moral conscience," adding that "the Supreme Court noted that in their
ruling." However, he cautioned that "there was disagreement about was this
means."23 Finally, he stated that there was "broad agreement" that physician
freedom of conscience "must be protected in a way that balances patients'
ability to access assisted dying."24
D2.2.6 Here he referred to four options for physicians who
refuse to provide euthanasia or assisted suicide, somewhat different from
those presented in the on-line consultation:25
1. Duty to refer directly to a non-objecting physician
2. Duty to refer to an independent third party.
3. Duty to provide complete information on all options and advise on how to
access directly a separate central information, counselling and referral
service.
4. Patient self-referral to a separate central information, counselling and
referral service.
D2.2.7 In listing the "pros" and "cons" of each, he
acknowledged that the third "may be the most widely morally acceptable
option," but warned that it presupposed the existence of a separate
counselling service - "a fairly large presupposition at this point in time."26
D2.2.8 The third option was a summary of what had been
proposed to the CMA by the Christian Medical Dental Society, the Federation
of Catholic Physicians Societies and Canadian Physicians for Life. The
groups urged delegates to accept it for the following reasons:
Options '1' and '2' require the objecting physician to refer. Many
physicians will have moral convictions that assisted death is never in the
best interests of the patient, while others may object to assisted death
because of the particular circumstances of the patient. A referral is
essentially a recommendation for the procedure, and facilitates its
delivery. A requirement to refer means that physicians will be forced to act
against their consciences.
Option '4' allows the patient to directly access assisted death, but does
not necessarily provide an opportunity for counselling by a physician who
has a longer term relationship with the patient.
Option '3' allows the discussion of all options to occur with the patient
and the physician who knows them. If, after considering all of the options,
the patient still wants assisted death, the patient may access that
directly. This option ensures that all reasonable alternatives are
considered. It respects the autonomy of the patient to access all legal
services while at the same time protecting physicians' conscience rights.27
D2.2.9 After a lengthy discussion, the third option was
approved in a straw poll, supported by about 75% of the delegates, who
agreed that "physicians should provide information to patients on all
end-of-life options available to them but should not be obliged to refer."18
D2.2.10 This account of the outcome is consistent with the
fact that only the first two options included a "duty to refer," while the
third did not. A further point, which would not have been apparent to
the delegates at the time, was that the outcome reflected the (undisclosed)
fact that 69% of survey respondents had indicated that they were opposed to
a requirement to refer to someone who would provide euthanasia or assisted
suicide (D2.2.3).
D2.2.11 The day after the delegates approved the third option
(a duty to provide information), Dr. Ken Burns and Dr. Shawn Whatley
proposed another resolution specific to referral:
The Canadian Medical Association policy on physician-assisted death will
reflect that physicians with consciencious [sic] objections should not be
obligated to refer for medical aid in dying. [Motion DM 5-60]28
D2.2.12 The rationale offered in support of the motion
repeated the kind of arguments made the day before:
CMA has indicated (survey and draft document) that referral is an acceptable
method to deal with a physician's conscience conflict. This not true for
many physicians. A forced referral (even through another party) for a
procedure they believe is wrong is not protecting conscience. CMA has
opposed the College of Physicians and Surgeons of Ontario's new policy but
appears to be backing down in its position. ' Council needs to decide
if it is going to protect even a minority of members' legal rights.
A very large number of CMA membership see any form of forced referral
against their conscience.They expect their organization to support their
fundamental rights.29
D2.2.13 However, after significant opposition from a number
of delegates, the motion was defeated, 79% of them voting against it.30
D2.2.14 The most likely explanation for this is the terminological problem that plagues discussion about "referral." It has a
technical meaning: a letter written by a physician to another physician
requesting treatment examination. It also has a popular meaning: some kind
of informal direction to a patient about where to obtain or how to find a
service or treatment. It is likely that many of the delegates who had, the
day before, approved the third option, considered it to be a form of
referral in the second sense. In that case, they likely rejected the
resolution because it appeared to them to contradict what they had approved
the previous day.
D2.2.15 Unfortunately, the rejection of the second motion
created the impression in some quarters that the CMA was opposed to
physician freedom of conscience. For example, Alex Schadenburg of the
Euthanasia Prevention Coalition reported that the CMA "voted to reject a
motion to protect the conscience rights of physicians who refuse to refer
patients to die by euthanasia."31 The
Western Catholic Reporter published a
story quoting Mr. Schadenburg under the headline, "Doctors to lose
conscience rights under CMA decision."32
D2.2.16 At their October, 2015 meeting, the CMA Board of
Directors approved Principles-based Recommendations for a Canadian Approach
to Assisted Dying as amended in consequence of the discussion at the Annual
' Council.33 The section on conscientious objection stated:
Physicians are not obligated to fulfill requests for assisted dying. There
should be no discrimination against a physician who chooses not to
participate in assisted dying. In order to reconcile physicians'
conscientious objection with a patient's request for access to assisted
dying, physicians are expected to provide the patient with complete
information on all options available to them, including assisted dying, and
advise the patient on how they can access any separate central information,
counseling, and referral service.34
D2.2.17 This was included the the CMA presentation on 20
October, 2015 to the panel
appointed by the federal government to report on the implementation of the
Carter ruling. The CMA offered the
following comments:
As the Federal External Panel is aware, the Carter decision emphasizes that
any regulatory or legislative response must seek to reconcile the Charter
rights of patients (wanting to access assisted dying) and physicians (who
choose not to participate in assisted dying on grounds of conscientious
objection). The notion of conscientious objection is not monolithic. While
some conceptions of conscience encompass referral, others view referral as
being connected to, or as akin to participating in, a morally objectionable
act.
It is the CMA's position that an effective reconciliation is one that
respects, and takes account of, differences in conscience, while
facilitating access on the principle of equity. To this end, the CMA's
membership strongly endorses the recommendation on conscientious objection
as set out in section 5.2 of the CMA's enclosed Principles-based
Recommendations for a Canadian Approach to Assisted Dying.35
D2.2.18 The section in the document concerning
conscientious objection was later modified by the Board of Directors.
The revision did not change the original section (in blue font below),
but added further details.
Physicians are not obligated to fulfill requests for assisted dying. This
means that physicians who choose not to provide or participate in assisted
dying are not required to provide it or participate in it or to refer the
patient to a physician or a medical administrator who will provide assisted
dying to the patient. There should be no discrimination against a physician
who chooses not to provide or participate in assisted dying.
Physicians are obligated to respond to a patient’s request for assistance
in dying. There are two equally legitimate considerations: the protection of
physicians’ freedom of conscience (or moral integrity) in a way that
respects differences of conscience and the assurance of effective patient
access to a medical service. In order to reconcile physicians’ conscientious
objection with a patient’s request for access to assisted dying, physicians
are expected to provide the patient with complete information on all options
available, including assisted dying, and advise the patient on how they can
access any separate central information, counseling, and referral service.
Physicians are expected to make available relevant medical records (i.e.,
diagnosis, pathology, treatment and consults) to the attending physician
when authorized by the patient to do so; or, if the patient requests a
transfer of care to another physician, physicians are expected to transfer
the patient’s chart to the new physician when authorized by the patient to
do so.
Physicians are expected to act in good faith, not discriminate
against a patient requesting assistance in dying, and not impede or block
access to a request for assistance in dying.36
D3. CMA rejects "effective referral"
D3.1 The Canadian Medical Association has continually
grappled with the issue of referral for morally contested procedures since
at least 1970, when the CMA Board of Directors decided that it would be
ethical for a physician to refer a patient to another physician for
consideration of an abortion, but not to an "abortion counselling agency."37
The difficult compromise eventually arrived at required objecting physicians
to disclose personal moral convictions that might prevent them from
recommending a procedure to patients, but did not require the physician to
refer the patient or otherwise facilitate the morally contested procedure.38
D3.2 It appears that the compromise was primarily a
pragmatic response to controversy. At any rate, the CMA did not offer
a principled ethical or philosophical rationale to support it, beyond
general references to the need to "strike a balance" between patient and
physician autonomy or rights. In 2014/2015, when the College of
Physicians and Surgeons of Ontario (CPSO) developed a policy requiring
objecting physicians to make an "effective referral," the CMA was notably
absent from the public controversy surrounding it.
An effective
referral means a referral made in good faith, to a non-objecting, available,
and accessible physician, other health-care professional, or agency. The
referral must be made in a timely manner to allow patients to access care.
Patients must not be exposed to adverse clinical outcomes due to a delayed
referral.39
D3.3 However, a crisis of sorts seems to have been
generated by the Carter ruling, as physicians awakened to its
implications for freedom of conscience and religion and even for the
legitimate diversity of clinical judgement. Within this context, the
perennially controversial issue of referral became more urgent, with
literally life or death consequences attached to it. Perhaps as a
result, the CMA has now issued a statement that articulates the basis for
its rejection of "effective referral," this time in response to CPSO plans
to impose "effective referral" for euthanasia and assisted suicide.40
Notes:
1. Canadian Medical Association Policy:
Euthanasia and Assisted Death (Update 2014)
(Accessed 2015-06-26).
2. Blackmer J, Francescutti LH, "Canadian Medical
Association Perspectives on End-of-Life in Canada." HealthcarePapers, 14(1)
April 2014: 17-20.doi:10.12927/hcpap.2014.23966
3. Canadian Medical
Association,
A Canadian Approach to Assisted Dying: A
CMA Member Dialogue Summary Report. (August, 2015)
p. 2 (Accessed 2015-10-23). (Hereinafter, "Summary Report").
4. Summary Report, p.2.
5.
Canadian Medical Association Annual General Council 2015,
Education
session 2: Setting the context for a principles-based approach to
assisted dying in Canada. Webcast- 13:40-13:45. (Hereinafter
"Ed2-webcast")(Accessed 2015-12-29)
6. Ed2-webcast - 15:00-15:22
7. Kirkey S.
"How far should a doctor go? MDs say
they ‘need clarity' on Supreme Court's assisted suicide ruling."
National
Post, 23 February, 2015
(2015-07-04)
8. In a 2014 poll of 5,000 CMA members, 27% of
physicians surveyed said they were willing to participate in assisted
suicide, while 20% were willing to participate in euthanasia. Assuming that
the results can be applied to the whole Association, that indicated about
21,600 physicians available for assisted suicide and 16,000 for euthanasia.
Moore E.
"Doctor is hoping feds will guide on assisted suicide legislation." Edson Leader, 12 February, 2015.
(Accessed 2015-07-16).
9. Ed2-webcast - 15:00-15:22
10. Ed2-webast - 15:23 - 15:39
11. Ed2-webast - 15:42 - 15:51
12. Assuming, (a) that those who would
provide euthanasia or assisted suicide for terminal illness make
up the 10% difference between 19% and 29% of the subset of
willing physicians, and (b) that those willing to provide
euthanasia and assisted suicide for psychological suffering
would also be willing to provide the services for the
non-terminally ill and the terminally ill, though the reverse
would not necessarily hold.
13. Ed2-webcast - 16:50-17:13
14.
https://www.cfpc.ca/uploadedFiles/Health_Policy/_PDFs/ePanel_psa_results_EN.pdf
15. Ed2-webcast - 17:20-17:25.
16. Ed2-webcast - 17:14-17:38.
17. Ed2-webcast - 17:38-17:55.
18. Picard A.
"Less than a third of doctors
willing to aid in assisted dying: CMA poll." Globe and Mail, 25 August,
2015
(Accessed 2015-10-22).
19. Kirkey S.
"Majority of doctors
opposed to participating in assisted death of patients: CMA
survey." National Post, 25 August, 2015.
(Accessed 2015-10-22).
20. Vogel L.
"Many doctors won't provide
assisted dying." CMAJ, 31 August, 2015
(Accessed 2015-10-22).
21. Ed2-webcast - 20:09.
22. Ed2-webcast - 15:53-16:22.
23. Ed2-webcast - 20:09-20:41.
24. Ed2-webcast - 20:41-20:50.
25. Ed2-webcast - 16:22-16:31.
26. Ed2-webcast - 22:29-22:50.
27. Christian Medical and Dental Society,
Doctors'
Group urges Canadian Medical Association to defend conscience rights on
assisted death. News release, 24 August, 2015
(Accessed 2015-10-23)
28. Canadian Medical Association,
148th Council Delegates' Motions -
End-of-life Care
(Accessed 2015-10-23).
29.
148th ' Council Delegates' Motions -
End-of-life Care.
Accessed 2015-10-23
30. Rutka J. "Conscientious objections, referral
for assisted dying prove controversial topics at CMA meeting ." Canadian
Health Care Network, 26 August, 2015
31. Schadenburg A.,
"Canadian Medical Association delegates
rejects conscience rights for physicians with regard to euthanasia."
(Accessed 2015-10-23).
32. Gyapong D.
"Doctors to lose conscience
rights under CMA decision." Western Catholic Reporter, 14 September, 2015
(Accessed 2015-10-23).
33. Canadian Medical Association,
Board of Directors October 2015 Meeting
Highlights (Accessed 2015-10-23)
34. Canadian Medical Association,
Principles-based Recommendations for a Canadian Approach to Assisted
Dying, Foundational Principle 2 (Accessed 2015-11-24).
35. Canadian Medical Association,
Submission to the Federal External Panel
on Options for a Legislative Response to Carter vs. Canada (Federal External
Panel) 19 October, 2015
(Accessed 2015-10-24)
36. Canadian Medical Association,
Principles-based Recommendations for
a Canadian Approach to Assisted Dying (2016) (Accessed 2016-01-09).
37. Board of Directors Meeting: "Therapeutic Abortion Study Major
Association Project: Finance Committee Reports Mild Optimism for Year." CMAJ
Volume 103(11) 1218, November 21, 1970.
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1930622/pdf/canmedaj01607-0085.pdf)
Accessed 2015-06-17
38. Murphy S.
"NO MORE CHRISTIAN
DOCTORS, Appendix 'F' - The Difficult Compromise. Canadian Medical
Association, Abortion and Freedom of Conscience." Protection of
Conscience Project
39. College of Physicians and Surgeons of
Ontario,
Professional Obligations and Human Rights (March, 2015)
(Accessed 2015-12-28).
40. Canadian Medical Association,
"Submission to the College of Physicians and Surgeons of Ontario: Consultation on CPSO
Interim Guidance on Physician-Assisted Death"(13 January, 2016)
(Hereinafter "CMA Submission")