A bureaucracy of medical deception
Quebec physicians told to falsify euthanasia death certificates
Regulators support coverup of euthanasia from families
Sean Murphy*
Full Text

In
the first week of September, the Canadian Medical Association (CMA) was reported
to be "seeking 'clarity'" about whether or not physicians who perform
euthanasia should misrepresent the medical cause of death, classifying death by
lethal injection or infusion as death by natural causes. The question arose
because the Quebec College of Physicians was
said to be "considering recommending" that Quebec physicians who provide euthanasia
should declare the immediate cause of death to be an underlying medical condition,
not the administration of the drugs that actually kill the patient.1
In fact, the Collège des médecins du Québec and pharmacy and nursing
regulators in the province had already made the decision. In
August, the three regulators issued a
Practice Guide directing
Quebec physicians to falsify death certificates in euthanasia cases.
The physician must write as the immediate cause of death the disease or morbid
condition which justified [the medical aid in dying] and caused the death. It
is not a question of the manner of death (cardiac arrest), but of the disease,
accident or complication that led to the death. The term medical aid in dying
should not appear on this document.2
Lawyer Jean Pierre Ménard correctly observed that Quebec's euthanasia
law does not require physicians to report euthanasia on death certificates.1
M. Ménard is an expert on euthanasia law consulted by the Quebec government
and the CMA,3
but he seems unaware of guidelines relevant to the classification of
deaths and medico-legal death investigations.
Those eligible for euthanasia in Quebec will be deliberately killed by the
sequential injection or infusion of three different drugs at a prearranged
date and time in accordance with detailed instructions provided in Practice
Guide. Only trained physicians will be allowed to administer the drugs.4,5
"Physicians want to avoid the 'horror stories' of botched executions in the
U.S.," explains Dr. Jeff Blackmer of the CMA,"or using wrong doses, or wrong
combinations of life-ending drugs."6
Particularly if the first course of drugs
fails, and the physician has to inject the second course to kill the
patient, the preparations and procedures described in the Practice Guide
more resemble an execution in the United States than death by natural
causes. Whether or not it is "botched", carefully planned and executed death
by lethal injection is not a "natural" death. At least, it certainly
does not appear to be natural.
Quebec physicians were formerly required by the
province's Coroners Act to report all
deaths that did "not
appear to be natural" to a coroner.7
Coroners determine the medical cause of death, classify it as death by accident, natural
causes, homicide or suicide, and report the cause and classification of
death on a death certificate.8 Other provinces have essentially the same
system.9
According to standard guidelines used across Canada, deliberately
killing a patient by lethal injection would be classified as
homicide.10,11,12
It would also homicide in criminal law.13
When the Carter decision takes effect or is enacted in statute,14 euthanasia
according to the terms specified by the Supreme Court of Canada will become non-culpable
homicide: homicide that is not an offence - but homicide nonetheless.15
The Quebec Coroner's Act was superseded by new legislation in 1986
which changed the reporting requirements, deleting the term "natural." Since
then, reports to a coroner or peace officer have been required from persons
other than physicians only if a death appears to be the result of "negligence or in obscure or violent circumstances" or if the identity of
the deceased is unknown. A different rule applies to physicians:
Every physician who certifies a death for which he is unable to establish
the probable causes or which appears to him to have occurred as a result of
negligence or in obscure or violent circumstances shall immediately notify a
coroner or peace officer.16

Return of Death
(SP3)(Physician)
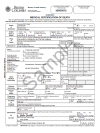
Coroner's Medical
Certification of Death
Homicide has always been considered a violent act, though only culpable
homicide is an offence, so the change in the law did not change the practice
with respect to the reporting and classification of deaths. As in
other provinces,
physicians' certificates of death (in Quebec, form SP-317)
are meant to be used only for death by natural causes. Coroners or
medical examiners use different death
certificates that include homicide, suicide and accidental death.18
Quebec's Act Respecting End of Life Care (ARELC) which purports to
legalize euthanasia by physicians, does not change the definition of
homicide or the distinction between homicide and death by natural causes.
However, it creates an anomalous situation with respect to the reporting of
deaths in Quebec because of the wording of the law governing reports to
coroners.16 A physician who kills a patient with a lethal injection or
infusion will certainly be able "to establish the probable causes" of death,
and is unlikely to believe that the patient died in "violent circumstances."
He can thus conveniently absolve himself of any duty to notify a coroner or
peace officer.
The anomaly could easily have been corrected, since the Quebec government
delayed implementation of the Act for 18 months to allow time to
bring other legislation and policies into line with it. That it has
not been corrected suggests that the Quebec government and regulatory
authorities are pursuing a policy of deliberate deception.
The result is a rather tangled web of contradictions that becomes evident when one considers
other direction given in
the Practice Guide:
Moreover, pursuant to paragraph 6 of section 3 of the Act Concerning End of
Life Care, only a physician can administer the medication to a terminally
ill person to obtain MAD. A physician is a person who holds a license and is
entered on the roll of the Collège des médecins du Québec. Thus, a student,
a medical resident or clinical monitor cannot perform this action, even
under supervision.19
It should be noted that, except as provided by law, aid in dying remains
subject to criminal sanctions.20
According to the logic of the Practice Guide, then, the killing of a patient by
lethal injection or infusion is a non-reportable death by natural causes at
the hands of a physician, but a reportable death by homicide at the hands of
a medical resident, even if the medical resident is acting under the direct
supervision of a physician in exactly the same circumstances.
This anomaly, however, exists only with respect to the reporting of
euthanasia deaths in Quebec. It does not affect the classification of
euthanasia deaths as homicide under criminal law or vital statistics rules.
That is straightforward. Assuming that all of the legal requirements have
been met in the kind of euthanasia case described in the Practice Guide,
it would be a simple matter to notify a coroner, who could easily establish
the cause and classification of death and complete a death certificate.
It is true that irregularities might cause a coroner to investigate the
circumstances at greater length, but one would expect a timely investigation
if there were irregularities, while witnesses and evidence are immediately
available. After all, the Practice Guide emphasizes that physicians
must "strictly" follow the law "to avoid unacceptable abuses,"21
and it indicates that a physician who provides euthanasia "except as
provided by law" is liable to be charged for murder or manslaughter.20
Nonetheless, the Practice Guide insists that Quebec physicians who
kill patients under the terms of ARELC are to falsify death certificates.
Jean Pierre Ménard argued that this may be justified to prevent next of kin
from discovering that a loved one was killed by a physician,1
and this is exactly the rationale offered by the Practice Guide.
First, it says, falsifying the cause of death makes it possible to respect
the wishes of patients who don't want their families to know how they died.
Second: it protects families who don't know that their loved ones have been
killed by physicians from unspecified "harm."22
It is this planned and deliberate deception by physicians that seems to have
unsettled CMA officials. Their uncertainty is understandable. They
take the position that physicians can have a professional obligation to kill
patients in circumstances defined by the Supreme Court of Canada.23 Since
killing is far more serious than mere deception, they may now be at a loss
to explain why physicians do not also have a professional obligation to lie.
Those who say that they do point out that euthanasia deaths in Quebec are
supposed to be reported to designated state agencies, so to the extent that
this is actually done, no "coverup" is involved. Falsifying death
certificates would not seem to constitute forgery if done in good faith, at
the request of the Quebec government through direction given in the
Practice Guide.24
Moreover, law professor Amir Attaran of Ottawa recently declared that
physicians cannot refuse to kill patients or help them commit suicide in the
circumstances defined in Carter. If judges and lawyers can
order physicians to kill patients, it would seem to follow that judges and
lawyers can order physicians to lie.25
On the other hand, the code ethics for Quebec coroners requires them to
act with "integrity, objectivity, rigorousness and independence,"26 while
the CMA Code of Ethics advises physicians to practise medicine "with
integrity"27 and to "resist any influences or interference" that might
undermine it.28 This suggests that falsifying death certificates would be
problematic for those who take codes of ethics seriously.
Certainly, physicians opposed to euthanasia have been upset by this policy
in the Practice Guide. The Physicians' Alliance Against Euthanasia has
deplored and denounced it publicly:
This instruction by the College is contrary to Article 19 of the Public
Health Act Regulation which stipulates that "the cause of death must be
indicated in the most accurate manner possible." It goes without saying that
such a practice constitutes a severe breach of ethics, and it will
inevitably lead to serious abuse, in addition to distorting the official
statistics on the real causes of death in Quebec.29
Many physicians, coroners and other health care workers may share these
concerns, even if they don't have moral reservations about euthanasia.
Indeed, euthanasia supporters may worry that mandating deceptive practices
is counterproductive and inconsistent with the Practice Guide's
expectation that physicians will apply "moral rigour" in processing
euthanasia requests.30
Others may be uncomfortable lying or dissembling to families about how
their loved ones died, which would seem to be unavoidably associated with
falsifying causes of death. They may be concerned that falsifying records
and lying to families is likely to undermine the trust essential to the
practice of medicine. And many people simply have moral or religious
objections to falsifying documents, lying, dissembling and other forms of
deception under any circumstances.
In addition, a good number of those who object to
euthanasia who are not directly involved in lethally injecting a patient will almost certainly consider
participation in deception to involve
unacceptable complicity in killing, even if it occurs after the fact. This
is not an unreasonable position. The killing of thousands of hospital
patients in Nazi Germany involved extensive falsification of death
certificates by physicians, supervised and assisted by state functionaries.
Their goal was to convince families that loved ones who had been lethally
injected or gassed had died from natural causes. Few would now say that
those involved in what Robert J. Lifton called a "bureaucracy of medical deception" were not morally
implicated in the deaths of those patients.31
The "clarity" sought by CMA officials might be found by reflecting upon
the position of the Collège des médecins du Québec and CMA
itself: that euthanasia
is a beneficial medical treatment. Beneficial medical treatments do not
require a bureaucracy of medical deception. Deception only increases the
likelihood of conflict and controversy.
Notes
1. Kirkey S.
"Medical leaders grapple with new euthanasia dilemma: What to write on the
death certificate." National Post, 4 September, 2015 (Accessed
2015-09-05).
2. "Le médecin doit y inscrire comme cause
immédiate de décès la maladie ou l'affection morbide ayant justifié l'AMM et
provoqué la mort. Il ne s'agit pas du mode de décès (arrêt cardiaque), mais
de la maladie, du traumatisme ou de la complication qui a entraîné la mort.
Le terme d'aide médicale à mourir ne devrait pas figurer dans ce bulletin."
Collège des médecins du Québec, Ordre des pharmaciens du Québec, Ordre des
infirmières et infirmiers du Québec, L'Aide Médicale à Mourir: Guide
d'Exercice (August, 2015), p. 49. Murphy S. "Quebec Euthanasia Guidelines:
Practice guide issued by Quebec health care profession regulators" (August,
2015) (parallel translation) Protection of Conscience Project,
T#198 -
T#201
(hereinafter "Guide")
3. Canadian Medical Association, Annual Meeting
and General Council, Education session:
Setting the context for a principles-based approach to assisted dying in
Canada (25 August, 2015) (Accessed 2015-09-05).
4. Ubelacker S.
"Quebec MDs to get euthanasia guide to prepare for legalized assisted death:Unclear whether other provinces and territories will adopt a similar
practice."The Canadian Press, 1 September, 2015 (Accessed
2015-09-03).
5. Guide, Chapters 4, 5, 6, Annexes III to IX.
6. Kirkey S.,
"Majority of doctors opposed to participating in assisted death of patients:
CMA survey." National Post, 25 August, 2015 (Accessed
2015-08-26).
7. "Whosoever knows or learns that a person died
suddenly or violently or from negligent or culpable conduct of some other
person, or from causes unknown or of a suspicious nature or which do not
appear to be natural, shall forthwith so inform the coroner of the district
where the body was found."
Quebec Coroners Act, Section 9 (Accessed 2015-09-05).
8. Statistics Canada,
The Coroner and Medical Examiner Systems. (Accessed 2015-09-05).
9. For example, among the kinds of deaths that
must be reported to a coroner, the Ontario Coroners Act includes deaths
"from any cause other than a disease."
Ontario, Coroners Act,
Section 10(1)f. (Accessed 2015-09-05).
10. "The cause of death variable in the CVS-D is
classified according to the World Health Organization's International
Statistical Classification of Diseases and Related Health Problems Tenth
revision (ICD-10)." Statistics Canada,
The
Collection of Death Data in Canada. (Accessed 2015-09-05).
11.
International Statistical Classification of Diseases and Related Health
Problems, Tenth revision (ICD-10), Vol. 2, 2nd Ed., 4.1.2: "It was
agreed by the Sixth Decennial International Revision Conference that the
cause of death . . . should be designated the underlying cause of death. . .
[T]he underlying cause has been defined as '(a)' the disease or injury which
initiated the train of morbid events leading directly to death, or (b) the
circumstances of the accident or violence which produced the fatal injury."
(Accessed 2015-09-05).
12. "Homicide - a death due to injury
intentionally inflicted by the action of another person." (Emphasis in
the original.) British Columbia Vital Statistics Agency,
Physicians' and Coroners' Handbook on Medical Certification of Death and
Stillbirth (2004 Ed.), p. 9 (Accessed 2015-09-05).
13. "A person commits homicide when, directly or
indirectly, by any means, he causes the death of a human being." Canada,
Criminal Code,
Section 222(1)
(Accessed
2015-11-15).
14. In February, 2015, the Supreme Court of Canada
struck down the law prohibiting physician assisted suicide and physician
administered euthanasia in circumstances defined by the court. The Court
suspended the ruling for a year to give the government time to respond
with appropriate legislation.
Carter v. Canada (Attorney General), 2015 SCC 5 (Accessed
2015-11-17)
15. Canada, Criminal Code,
Section 222(3)
(Accessed
2015-11-15)
16. Quebec,
Chapter R-0.2,
An Act Respecting the Determination of the Causes and
Circumstances of Death, Section 34
(Accessed 2015-11-15).
17. Gouvernement du Québec, Ministère de la
Santé et des Services sociaux,
SP-3,
Return of Death
(Accessed 2015-11-15)
18. For example, For example, British Columbia,
Ministry of Health Planning, British Columbia Vital Statistics Agency,
Coroner’s Medical Certification
of Death.
19. "D'ailleurs, suivant le paragraphe 6o de
l'article 3 de la Loi concernant les soins de fin de vie, seul un médecin
peut administrer le médicament permettant à une personne en fin de vie
d'obtenir l'AMM. Un médecin est une personne qui détient un permis
d'exercice et qui est inscrite au tableau du Collège des médecins du Québec.
Ainsi, un étudiant, un résident en médecine ou un moniteur clinique ne peut
pas effectuer ce geste, même en étant supervisé." Guide, p. 23-24;
T#106 to
T#108
20. "Il est à noter que, en dehors des
conditions prévues par la Loi, l'aide à mourir demeure passible de sanctions
criminelles." Guide, p. 12 (T# 022)
21. "Pour éviter des dérives inacceptables, le
législateur a encadré sévèrement le processus décisionnel habituel en
imposant des conditions, à la fois d'ordre juridique et d'ordre clinique
(art. 26 et 27), et en exigeant des procédures que les médecins doivent
suivre strictement (art. 29)." | "To avoid unacceptable abuses, legislators
severely restricted the usual decision-making process by imposing
conditions, both legal and clinical, (art. 26 and 27), and requiring
procedures that physicians must follow strictly (art. 29)." Guide, p. 13 (T#
028)
22. "En effet, une telle mention, si elle était
connue de proches non informés, pourrait d'une part aller à l'encontre de la
volonté d'un patient souhaitant garder ce renseignement confidentiel et,
d'autre part, leur causer préjudice." | "Indeed, such mention, if it became
known to uninformed relatives, could firstly go against the will of a
patient wishing to keep this confidential information and, secondly, cause
them harm." Guide, p. 49-50 (T#201)
23. Canadian Medical Association Policy:
Euthanasia and Assisted Death (Update 2014) (Accessed
2015-06-26)
24. Canada, Criminal Code,
Section 366(5). Forgery is defined as knowingly making a false document
with the intent that someone, believing it to be genuine, should do or
refrain from doing anything. However, the law makes an exception for those
who make false documents at the request of the police, military or the
federal or provincial government. (Accessed 2015-09-05).
25. Attaran A.
"Doctors can't refuse to help a
patient die - no matter what they say." iPolitics 13 November, 2015
(Accessed 2015-11-17).
26. Quebec,
Code of Ethics for Coroners, Sections 10, 15 (Accessed 2015-09-05)
27. Canadian Medical Association,
Code of
Ethics (Update 2004), 5
28. Canadian Medical Association,
Code of
Ethics (Update 2004), 7
29. The Physicians' Alliance Against Euthanasia,
"The College of Physicians promotes secrecy in its practice guideline for
"medical aid in dying" (23 September, 2015)
(Accessed 2015-11-15),
30. "Il reste nécessaire que les médecins les
suivent avec bon sens et rigueur morale." | "It remains necessary for
physicians to apply common sense and moral rigor." Guide, p. 13, (T#027)
31. Lifton R.J. The Nazi Doctors: Medical
Killing and the Psychology of Genocide. New York: Basic Books, 1986, p.
74-75